Recently, on Goodreads, a reader wrote a very thorough review . . . It makes me think I should just do a book of all of “Dede’s Grey Boxes” from the Crohn’s book! What do you all think? A “how-to” from a patient who has kicked Crohn’s disease? A “saying no” to major medical institutions (like the Mayo Clinic) who advised me to start medication (Remicade/Humira, etc.) immediately and I didn’t and I beat the disease by following a naturopathic/holistic health plan that was outlined in our book . . . (just to be clear: Allopathic medicine saved my life by a combination of prednisone and bowel surgery of my small and large intestine (about 2 feet) to keep me alive…)
Check out the review & Happy Spring! Maybe I will work on this new book if it will help people!
~Dede
Living with Crohn’s & Colitis: A Comprehensive Naturopathic Guide for Complete Digestive Wellness
by Rebecca
Recommended for: People with Crohn’s, Colitis, IBD and their loved ones
Having just had a bad flare up of my Crohn’s, and a long and scary stay at the hospital, I’m now on a mission to read up more on current healing and overall wellness for people in my situation. This book was the only one amongst a sea of books that I had any interest in reading as a jumping off point. The combination of medical and personal account in this book is incredibly helpful. Hearing accounts of those who have “been there, done that, got better!” really is a spirit lifter for someone coming out of a bad flare and wanting to get on the right path.
The clinical information in this book is spot on and seems highly up to date. The biggest part of which is the proliferation of the idea that diet does matter to this disease. I was utterly dumbfounded during my hospital stay when I was given a menu of items I was allowed to eat (after being off food nearly a week) and it included so much junk. Though I didn’t thoroughly question my multiple doctors on their stance of diet in relation to Crohn’s, I got the impression most of them are operating under the “it doesn’t really matter what you eat” mentality. This blind spot in medicine, and not just related to Crohn’s, is a huge failing of our current system, and getting doctors to work with you on natural healing can be a challenge. Thankfully, books like this one are out there to help people start to see the interconnectedness of things like food, stress, supplements, along with pharmaceutical drugs and “modern” medicine. I have to give this book 5 stars for being detailed but understandable, informative, up to date accurate, and personally relate-able. The tips and tricks through the book are easy to understand and begin to incorporate in a healing plan for yourself. I recommend keeping paper and pen nearby to write down the names of various healing methods to try (like acupuncture and massage), as a reminder to look up that sort of thing in your area, and write down the names of supplements, foods and meals to try, etc.
My only complaint about this book is that Dede’s story and a lot of the helpful information is incredibly scattered throughout the book. We get chunks of things here and there between the related medical information. It was fine when reading through the first time, but I think the book would benefit from a few sections at the end that sort of combine the snippets scattered throughout into a more cohesive “summary” type section at the end for easier access when you want to use this as a reference instead. This is truly minor though, and since I can easily search the book on my Kindle it isn’t a huge deal to go back to re-read.
This book is a most excellent jumping off point for anyone wanting to get more information about Crohn’s and Colitis and a path to begin healing the whole body, not just covering up symptoms.
~~~

When you or your loved one was first diagnosed with IBD, you probably felt like your life and taking a sudden spiral downward. You may have found yourself in the state of utter confusion, a deep-seated feeling of loneliness and depression taking root in the very core of your being. This may sound dramatic, but too many sufferers of both Crohn’s disease and ulcerative colitis feel this way in response to their diagnosis. The good news is that the better informed you become about your newly diagnosed condition, the better off you will be in the long run.
One problem that many people with IBD know all too well, is that these diseases, especially Crohn’s disease, can reoccur. Although therapies can reduce signs and symptoms, often the hope for full remission is stymied by widely varying factors.
Treatment options often include hospitalizations, surgery, and medications, but they rarely include a holistic approach that incorporates acupuncture, a new diet (potentially wheat-and-dairy-free), stress reduction, psychotherapy, yoga and meditation, naturopathic medicine, and a special protocol in detoxification.
When the proper groundwork is set for healing, the treatments, lifestyle practices, and even pharmaceutical medications, are much more effective at reducing symptoms and promoting healing. Our bodies were meant to function as a whole, and treatment plans should always be directed at the whole body to achieve the desired effect of wellness.
For me, as a Crohn’s disease patient, I benefit so much from going to see my regular doctor (an M.D.), and my naturopath (and ND), as well as my IBD specialist at the clinic at Dartmouth. I hope that someday soon, all three will be able to work together seamlessly. Until that time, I have to be the instigator, and make sure that my medical records are sent to all three places, and I have to be very proactive to stay on top of my appointments, asking my questions, doing my own research, and creating my own support system. All of the specialists and doctors are very busy people (as most of us are), and it is imperative for those of us with IBD, or our caregivers, to be very motivated.
Sometimes it can feel overwhelming. But make a list of things to do:
- Walk every day—start small, and gradually add miles. . . . A walk on the beach, like my friend in the photo, really releases stress. Do a short yoga stretch before or after!
- Buy a new water bottle—I love my 22-ounce LifeFactory glass water bottle with the rubber exterior!), and take one step at a time.
- Find a recommended naturopath in your area.
- Make sure you have at least yearly appointments with all the doctors on your “team.”
- Embark on the new dietary guidelines in this book.
- Take a high-potency probiotic (I take 1 capsule daily, called VSL#3, that really seems to be helping by bowel movements), or one that is recommended by your team.
- Consider asking your MD or ND to do a complete blood work-up, and also to test your adrenal function.
- (Last, but not least,) Work with a naturopath, preferably, to balance the immune system to achieve homeostasis that is promoting wellness in your mind and body.
Happy Spring Detox and Motivation….. And Happy Almost Summer!
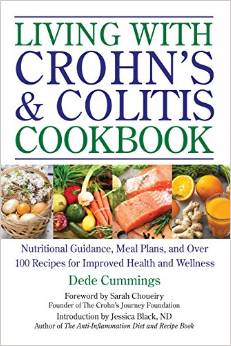 Our new cookbook is out and Dede would like to give away a free copy to the first two people who comment on this post — tell us a bit about yourself, are you a caregiver, do you have Crohn’s, or colitis, or IBS, or some other autoimmune disease? When you receive your book (send email in PM to dede@livingwithcrohnsandcolitisbook.com), please post a review on Amazon for us and we will be eternally grateful!
Our new cookbook is out and Dede would like to give away a free copy to the first two people who comment on this post — tell us a bit about yourself, are you a caregiver, do you have Crohn’s, or colitis, or IBS, or some other autoimmune disease? When you receive your book (send email in PM to dede@livingwithcrohnsandcolitisbook.com), please post a review on Amazon for us and we will be eternally grateful!
We are excited to share these gut-friendly recipes from the book and there is a long introduction about how to live with IBD and tips to help.
For the millions of people afflicted with irritable bowel disease (IBD), including Crohn’s and colitis, it can be a daily struggle to find nutritious meals that won’t aggravate symptoms or cause a flare-up. The Living with Crohn’s & Colitis Cookbook is your essential nutrition guide with over 100 recipes and meal plans expertly designed to improve daily functioning and help relieve symptoms of Crohn’s and colitis.
The Living with Crohn’s & Colitis Cookbook contains everything you need to plan your meals, balance your diet, and manage your symptoms, including:
• A guide to keeping a food journal
• Sample meal plans
• Tips for shopping for an IBD diet
• Gentle and nutritious recipes to help soothe flare-ups
…and much more!
The Living with Crohn’s & Colitis Cookbook features over 100 recipes, including Zucchini Buckwheat Banana Bread, Homemade Almond Milk, Dr. Lang’s Healing Soup, Garlic-Herbed Scallops, Coconut Curry Chicken over Brown Rice, Mushroom Risotto with Cashews and Parmesan, Crabapple Walnut Cake, and many more. The book also features Paleo recipes.
Enjoy these photos from our book!
Switching to a diet high in Omega-3s has been a major factor in my being in remission!
When I was first diagnosed with Crohn’s and colitis, I did not exactly jump into the fray of changing my diet and lifestyle… It took a few years! When you set out to try to change habits that are ingrained and also are associated with comfort (mother’s mac ‘n cheese anyone?), it takes time.

Wild-caught salmon follows the seasonal run of the Pacific Northwest. Photo courtesy of Central Mkt.
Now that I am on the other side of my twenty-year Crohn’s/colitis saga, I am in a place where I want to help others find their own way.
Once thing I have learned through my dietary study, is the fact that we need Omega-3 fatty acids in our diet daily—and not just if you are a Crohnie or uc-er. Every day.
I eat wild-caught salmon at least once a week, take flax seed ground up to aid in digestion and add fiber to my diet. I also take an Omega-3 supplement daily that really helps my arthritic joints (due to Crohn’s). I am healthy, fit and the doctors are surprised and how well I am, relying on diet, supplements and a holistic lifestyle.
Someone like me would normally be on autoimmune suppression drugs, but I do not want to do that to my body, and my choice was a wise one as I am incredibly healthy!
Omega-3 fatty acids are found also in walnuts, which I also eat every day. Other sources are the ALA (alpha-linolenic acid) Omega-3 fatty acids found in certain vegetable oils like soybeans, canola and flaxseed, as well as in green vegetables (kale, and more kale!, spinach, Brussels sprouts, and leafy greens). The other type of Omega-3 fatty acid is called EPA (eicosapentaenoic acid), and is present in salmon especially, as well as other types of fatty fish: Bluefish, mackerel, herring, tuna, anchovies and sardines are also excellent sources of omega-3s.
According to Dr. Frank Sacks, Professor of Cardiovascular Disease Prevention, Department of Nutrition, Harvard School of Public Health, you should have at least one serving of Omega-3 fatty acids in your diet daily.
In my upcoming cookbook, Living With Crohn’s & Colitis Cookbook: A Practical Guide to Creating Your Personal Diet Plan to Wellness (with an Introduction by Jessica Black, ND, and a Foreword by Sarah Choueiry, Crohn’s patient and founder of The Crohn’s Journey Foundation) due out in September (!), I have a few salmon recipes, and I’d like to share one now (quick and easy and great for summer dining—remember, if one of the foods, like apples, is a trigger food and hard to digest, substitute it or delete it from the recipe and adjust the mayo and seasonings accordingly)…. Enjoy!
Easy Salmon Salad
Ingredients:
2 cans wild boneless, skinless salmon
½ cup mayonnaise, organic
½ cup minced carrots
½ cup minced apples
¼ cup sweet relish, organic and sweetened naturally
Directions:
Mix all ingredients in a large bowl. Serve chilled with crackers, on a salad, or alone.
Source: http://www.hsph.harvard.edu/nutritionsource/omega-3/
….and I also want add a checklist for how to shop for the best salmon and how to cook and store the fish, as follows:
Wild-caught salmon (in photo) follows the seasonal run of the Pacific Northwest, and we strive to be first to market. According to the folks at Central Market, you should only buy from markets that buy fish from strictly regulated fisheries committed to sustainable practices and the guidelines set forth by the Marine Stewardship Council (MSC). The fish has been out of the water less than 48 hours prior to its arrival, flown in fresh several times a week and each piece is inspected.
Here are some tips from them to best enjoy your wild-caught salmon:
- Eat or freeze within 24 hours. Keep it in the refrigerator covered tightly in plastic wrap until you’re ready to cook it.
- Don’t rinse with water or the color will leach.
- If grilling, preheat grill to medium-high and grease it well with olive or grapeseed oil. Place the salmon on the grill, meat side down, and cook for 3 to 4 minutes, depending on thickness of the fillet. Flip over and cook 3 to 4 minutes more, skin side down. Also try it with a cedar plank. Sear with meat side down, then place skin side down on cedar plank and close the grill to infuse that cedar-smoked flavor.
- If using a cast-iron skillet, heat it until almost smoking and sear 2 to 3 minutes on each side. Pull it off the heat and let it continue to cook in the skillet until desired doneness.
- Salmon is done when it starts to flake, and it tastes best with a medium center.
Now that you know how to store and prep your salmon—enjoy! You can also pre-order my cookbook right here at your local, independent bookstore, and Sarah Choueiry and I are really excited to introduce you to a ton of great and easy recipes!
Happy Almost Summer!
I found this photo this morning, when I was remembering how scared I was going in for surgery for a bowel resection due to a serious, three-week, blockage of my small intestine from complications of Crohn’s disease.
I only weighed 117 pounds in this photo, taken with my son’s college roommate, Justin, two days before my operation in 2006. I was so skinny and malnourished, it’s hard to believe now that I am over twenty pounds heavier! I also found my husband’s post on my CaringBridge site (which still exists under “DedeCummings”), and I want to tell all my readers and followers of this blog, that you should never give up hope!
Written May 22, 2006 8:35pm
Hi all–
The news from Hanover is very good: Dede was in surgery from about 9:30-noon, and awoke (in a manner of speaking) about an hour later. She had a good grip on the button of her morphine pump, and smiled beatifically every time she heard its answering “beep.”Dr. Henriques took out approx. 5 inches of her small intestine, of which 5 cm had severe scarring and the rest was worn out, and about the same length of large intestine, which had been scarred by a fistula (an “abnormal passage” connecting the two, resulting from her disease/scarring). The doctor held up his index fingers like a fisherman describing his catch when describing all of this.
He also took out her appendix while he was in there, so we’ll have no access to supplementary information about her internal organs in the future. (Sorry: lame book joke…) Her gall bladder looks fine, just for the record.
He expects her to be in the hospital for only a few days, so she could get home as soon as Thursday. She has already gotten out of bed, taken a few steps, and sat up for a while.
By tomorrow she’ll be treated to smoothies and milkshakes, and can eat some solid food by the end of the week–Dr. Henriques predicts that she’ll be voracious by that point.
Thanks for all of your lovely notes and positive thoughts; I’ll be able to get my computer online in her room tomorrow, so keep ’em coming.
In some human diseases, the wrong mix of bacteria seems to be the trouble.
I recently discovered a new blog that is specifically for Chronic Fatigue Syndrome and Fibromyalgia. It is called Health Rising and the link is below.
There are articles that explore gut health and microbiota by Ken Lassesen, that really explain the importance on overall homeostasis for everyone, whether you have Crohn’s, colitis, IBS, IBD, Celiac, etc.
I am on a strict diet of no dairy, no grains, no sugar. Supplements include probiotics and turmeric. I am really healthy and haven’t had symptoms for almost eight years! I did have a partial bowel resection, in 2006, that changed my life and set me on a path toward wellness— that is when I wrote my book because I was disillusioned by the recommendations of my GI doctors who said I should take heavy-duty, autoimmune-suppressing drugs.
Read more: Bacterial Resistance, Infection and Chronic Fatigue Syndrome: Fighting Infections Pt. I http://www.cortjohnson.org/blog/2014/03/26/bacterial-resistance-infection-chronic-fatigue-syndrome-fighting-infections-pt-1/
~~~
~
In some human diseases, the wrong mix of bacteria seems to be the trouble, Part 2.
A recent NPR story on gut bacteria and Crohn’s disease really impressed me, so I want to share it in its entirety here on my blog!
Mix Of Gut Microbes May Play Role In Crohn’s Disease
The particular assortment of microbes in the digestive system may be an important factor in the inflammatory bowel condition known as Crohn’s disease.
Research involving more than 1,500 patients found that people with Crohn’s disease had less diverse populations of gut microbes.
“[This] basically for the first time identifies what might be the bacterial changes in patients with Crohn’s disease,” says Ramnik Xavier, of Masssachusetts General Hospital in Boston, who led the work.
More than a million Americans suffer from Crohn’s, which seems to start when an overreactive immune system causes abdominal pain, diarrhea, bleeding, weight loss and other symptoms. Many patients have to take powerful steroids (which can have serious side-effects), and some have parts of the digestive tract surgically removed.
Mounting evidence has suggested that microbes living in the gut might contribute to the problem. So Xavier and his colleagues compared the species of bacteria in more than 447 Crohn’s patients to the mix of microbes in more than 221 healthy people.
In their paper published in the journal Cell, Host and Microbe, the researchers detailed the clear difference they discovered: The patients with Crohn’s seemed to have too many of the sorts of bacteria that rile immune systems.
In addition to having less diversity in their gut microbes, Xavier says, the Crohn’s patients had fewer bacteria that have been associated with reduced inflammation and more bacteria associated with increased inflammation. (The findings were confirmed in 800 Crohn’s patients from other studies.)
Interestingly, children whose doctors had tried to treat their Crohn’s symptoms with antibiotics before they were properly diagnosed had a mix of microbes that was the most out of whack.
“We may have to revisit the use of antibiotics in [these] patients with early-onset Crohn’s disease,” Xavier says.
Instead, doctors might eventually do better to identify and prescribe treatments that mimic the helpful bacteria, he says, along with foods or other pharmaceutical agents that reduce or counteract the harmful bacteria.
“There’s the possibility that we might be able to identify [some] sort of super-probiotics that might be able to correct the gut back to the healthy state,” Xavier says.
UCLA pathologist Jonathan Braun, who studies microbial ecology, says the paper offers important first insights into illnesses beyond Crohn’s. “Other diseases are thought to be driven at least in part by bacteria,” he says, such as some inflammatory and autoimmune disorders. Bacteria may also be involved in obesity.
Humans should work harder to understand bacteria, Braun says, “and live with them when they’re helping us, or get them to serve us better when they are causing harm.”
~
Good for the media to pick up in the importance of balance in the flora and fauna of the gut—remember, everyone is different and there is no know cure for Crohn’s (for UC, the large colon can be removed, putting the patient in remission, but that is not the case for Crohn’s unfortunately).
So, with Spring on the way, now is the time to set some goals for health: sign up for Team Challenge with the Crohn’s and Colitis Foundation of America, walk 3 miles a day (get your heart rate up by walking up hills), do yoga/meditate, get lots of sleep, make an appointment with a naturopath, too. Spring brings with it hope for new life (and here in Vermont, lots of mud!).
I would definitely recommend getting another opinion. I got two!
One of our readers wrote to say her doctor told her she “shouldn’t feel any pain from UC.”
Seriously?
Pain is a bi-product of both Crohn’s disease and ulcerative colitis. My disease caused pain when I flared—it even felt like labor pains! I have Crohn’s. My disease is characterized by scarring—called fibro stenotic disease. UC does not usually go through the outer wall of the large intestine the way Crohn’s does with the small… So some people don’t have pain, but have diarrhea instead.
Remember, everyone is an individual, and we have different symptoms and react differently to different foods, or stress, for example. I (Dede) always say this: listen to your own body, ease off on trigger foods, like dairy or wheat, be proactive in your health care and do research and ask questions. Bring a list, and a partner or a friend, to your doctor’s appointments.
One time, I brought my husband, and he had done all this research (he’s an English professor ;)… at one point in the meeting, the gastroenterologist leaned over his desk and said to my husband, “Hey, what do you have on that drug?”
One thing to be aware of: getting off Prednisone. Did your doctor tell you to taper off slowly? My GI did. I love my team at Dartmouth Hitchcock in NH, it’s important to find a clinic and doctor you can trust who really listens to you!
Diet—yes, can cause pain and symptom flares. Don’t let a doctor fool you! Listen to your own body!
There is an excellent website-forum called www.ihaveuc.com and you should “tell your story,” and pose any questions you have there, also.
Greetings from Vermont. I am the co-author of Living With Crohn’s & Colitis: A Comprehensive Naturopathic Guide for Complete Digestive Wellness (with a nationally-known naturopath, Jessica Black, ND). Our book has helped so many people afflicted with Inflammatory Bowel Diseases, part of the growing auto-immune diseases that cause diarrhea, bloating, nausea, vomiting, and cramping. These inflammatory bowel diseases, and other auto-inmmune disease are on the rise exponentially across the world, especially in the developed countries where processed food is available.
Think about it: There are certain behaviors that cause body/mind stress: We address this in the book, but I want to tell you that I am a patient/survivor of a stress-induced flare-up in 2006 that almost killed me. On my 5 foot 8 frame, I weighed 117 pounds. I spent a month at Dartmouth Hitchcock Medical Center. I was 45 and very sick, with 3 children at home and a business to run.
Stress was the way I worked, and I was on autopilot without taking time for myself. That has all changed, and I have been in clinical remission for the last 7 years! Let me tell you more….
As many readers know, I went to the Mayo Clinic in Rochester, Minnesota this past May to have a complete second opinion. I spent two days of my weeklong stay, at the wonderful stress reduction clinic.
~
Here are some of my tips gained from my research, and how I try to keep my disease in remission:
STRESS
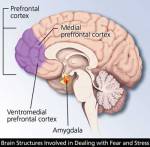
 A lot of us have low level stress. Most of us don’t live in the hyper-aware world, and we suffer the autopilot behaviors that contribute to what I call “the slow burn of stress response.” Our heart rate and blood pressure might be elevated, and our breathing and muscle tension is like this — shallow breathing and knots in muscles. There is an area at the base of the brain called the amygdala. This is the seat of our emotional reactions, or “flight of fight” response to stress. Many Americans live with this elevated, but low level elevation daily… a little bit of “Flight of Fight” stress is really okay, but not on autopilot.
A lot of us have low level stress. Most of us don’t live in the hyper-aware world, and we suffer the autopilot behaviors that contribute to what I call “the slow burn of stress response.” Our heart rate and blood pressure might be elevated, and our breathing and muscle tension is like this — shallow breathing and knots in muscles. There is an area at the base of the brain called the amygdala. This is the seat of our emotional reactions, or “flight of fight” response to stress. Many Americans live with this elevated, but low level elevation daily… a little bit of “Flight of Fight” stress is really okay, but not on autopilot.
Look at our brains — In our pre frontal cortex, there is an area responsible for relaxation, and it is not easy to stimulate and not an adrenal release, as per the amygdala part of the brain.
~
First we need to be aware of this pre frontal cortex We have to explore our own behaviors and habits, break out of autopilot, and participate in a personal practice. There are some things you can’t control, like weather or traffic jams; however there are some things we can control, and are important… An example from the workshop was if you have an overbearing mother (don’t worry, Mom, not YOU!), and how you need to take care of yourself first and use the excuse of health, and scale down. Awareness helps, and limit your exposure to stressful people and situations. It’s a process… keep boundaries in your mind, but “caring boundaries.”
Unhealthy responses to stress in our life are anger, etc. It is important to develop a healthy exercise routine, learn and use relaxation techniques (see below), and take care of yourself. This neural pathway gets easier and easier to tap into (see diagram at right). For example, my body knows and relaxes immediately when I walk into my home “yoga area” where I have a TV, and a carpet with a yoga mat. I use Rodney Yee’s DvD, “AM/PM Yoga,” and do the exercises every day… it gets easier and easier to tap into the relaxation part of my brain, and it is replenishing.
After a stressful day:
- Call a friend
- Laughter
- Read a book
- Knit
- Walk
- Walk the dog
- Ride a horse
- Volunteer at a soup kitchen
- Play the piano
- Do some gardening
In order to break out of autopilot, do a few things on this list on a regular basis.
~
Benefits: Concentration, Problem solving, Sleep…
We need to be participants: This involves “letting go of the wheel,” loosening your grip, and takes time and experimentation.
In the wonderful workshop, our instructor gave the analogy of flying on an airplane, and how you put the oxygen mask first, then help the child.
Talk therapy is another way to help relinquish the autopilot lifestyle… A regular monthly session with a trained, recommended therapist will do wonders for helping to care for yourself, establish boundaries, and feel safe.
Evaluate your stressors and prioritize your time, as you move forward in the break from autopilot.
Give yourself permission eg., “Be kind to yourself and ask for help.”
Often we don’t think about our career as a choice made for healthy reason, and it might be time to reevaluate what we do for work.
It is important to spend time with friends, develop hobbies…. Hanging out with people who make me laugh is a goal. A hospital study involved a control for two groups with the same malady: One group watched funny movies every day, and got out of the hospital faster.
It’s a process, and it is important to practice positive self talk.
—-
Start a simple practice of Tai chi and chi gong
Walk around with a gentle smile on your face and try to share it with strangers—you use less muscles and tension when you are not frowning, which can contribute to an overall sense of well-being and a way to focus on releasing the internal stress caused by being on autopilot…
I have found this “small smile” technique that is practiced by Amit Soud, MD, the head of the Eastern Medicine Section of the Mayo Clinic to be essential as a way to lessen internal stress.
~
TAI CHI AND CHI GONG: These ancient exercises are easy and relaxing, often available in small towns across the United States. For example:
We breathe with about 40% of our lungs. If we can learn to take slow diaphragmatic breaths, we can effortlessly lesson our stress levels. These exercises are the foundation and essential for relaxed breathing.
A simple exercise I learned at the Mayo Clinic:
Take in a slow deep breath,
and fill your lungs so even your belly sticks out;
hold for a couple of seconds;
pretend you have a lit candle and exhale
so that the candle flickers.
Note to reader: it might take 8 weeks or so to start seeing results.
 A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
Crohn’s is not easily deterred. I was so lucky to have seven years of clinical remission. It was only in the last year, that my disease spread. My last seven years have been filled with hope and health, and it is easy to fall into despair when the doctors tell you that your disease has gone from nonexistent to “severe.”
~
Rather than saying “Woe is me,” and spending time feeling sad and useless (I did a lot of that, believe me), I decided to take action, and try to live the words of the Dalai Lama:
“Scientists say that a healthy mind is a major factor for a healthy body,” His Holiness said. “If you’re serious about your health, think and take most concern for your peace of mind. That’s very, very important.”
That said, I am on my way to health, for sure—no time to sit on my cushion meditating (I do that daily for a few minutes still); rather, I need to stay focused and take care of my body: better food, sleep, stress relief, education, awareness, team building, satisfying work, making money enough to live on, giving back to my community and the world…working for peace, justice, and environmental sustainability. According to His Holiness the XIV Dalai Lama, peace of mind is essential for health—words to live by.
This new diet, very much like The Paleo, is giving me strength and vitality. It is not for everyone—and I always tell people you must proceed with a doctor’s knowledge, for Crohn’s and UC can be serious, even fatal, if not managed correctly. I have worked really hard to form a collaborative team—my own book’s co-author, Jessica Black, ND, is my stalwart supporter and her book, The Anti-Inflammation Diet and Recipe Book has just come it in a second edition and has sold almost 100,000 copies! Jessie is an amazing health practitioner.
~
I have eliminated ALL grains and dairy from my diet—woohoo! What a difference. I found this great site, and I can use almond meal flour (also coconut flour), and I eat fruits and veggies, nuts and animal protein pretty much non-stop. I had an adjustment for the first week, as I really missed my oatmeal in the morning, but as you can see from the photo, my morning meal is wonderful and tasty, too.
I hope this post inspires people to look at their own diets, and proceed with caution (this diet is not recommended if you have flare-up symptoms of Crohn’s or ulcerative colitis). I began this diet with no symptoms, and after the first week, I started to feel like I had more energy, and my stress levels are kept low by walking 4 miles a day and sleeping 8 hours per night.
I’ll post some more photos of my wonderful meals… Summer is the best time to do this diet: only organic fruits and veggies and meat must be antibiotic-free, grass-fed…that whole thing! I buy all local meat, eggs, fruits and veggies… And I plan on putting up and preserving a lot of them this summer so I can continue summer’s bounty from my freezer (and canning room) during the cold Vermont winter!
I also have a nice little garden growing…. Kale, and more kale! Plus, tomatoes, green beans, lettuce, spinach, onions, asparagus, etc. growing your own food is another way to reduce stress and get physically fit—gardening is good for upper body strength!
Inflammatory Bowel Disease (Crohn’s & Ulcerative Colitis)
Our first-ever “guest post” on Dede’s blog! Drew and I “met” through Dede and Jessica Black, ND’s Facebook page, and Dede invited him to educate our readers and followers about the benefits of accupuncture. WTG, Drew! This is like a new book we should publish! A very thorough examination of signs and symptoms of Crohn’s and ulcerative colitis, along with specific treatment plans for acupuncture. Since Dede (seriously) is a wimp when it comes to needles (also, working on this using Ayurvedic treatment to help with this possible symptomatic “sensitivity” on the skin, which is very likely bowel, related, since the skin and the bowel ARE related!~)…Please welcome Drew, and share this, and come visit him if you live in the Southern California region—like our friends at the CrohnsJourneyFoundation.

This happy woman is like Dede, who hates needles, but has monthly acupuncture treatment—it really helps alleviate symptoms and detoxify the overworked liver, etc. when you have an auto-immune disease
Inflammatory Bowel Disease is a heading/umbrella that has other diseases underneath it. You may have heard of Crohns Disease, Ulcerative Colitis and Irritable Bowel Disease. You may know someone who’s been diagnosed with one of these or you may have had one of these unfortunate afflictions. In any case these can be serious debilitating conditions that sometimes require extreme care for severe cases but all require long term care. In this article I will discuss the differences and similarities between the three.
Crohn’s Disease: A chronic inflammatory condition of the intestinal tract was first described by Dr. Burrill B. Crohn in 1932, along with Dr. Leon Ginzburg and Dr. Gordon D. Oppenheimer. Mostly affects the end of the small intestine called the “Ileum” and the beginning of the colon/large intestine “Cecum” but can affect the entire length of the GI tract. Crohn’s disease can affect the entire thickness of the bowel wall leaving “skip lesions;” whereas, Ulcerative Colitis only affects the superficial layer of the large intestine.
Ulcerative Colitis: A chronic inflammatory disease that affects only the Large Intestine (aka: colon). The lining of the colon becomes inflamed, and ulcerations occur which bleed and produce pus.The inflammation and the ulceration lead to spasms, cramping/pain and frequent bowel movements.
Like Crohn’s Disease Ulcerative Colitis is an autoimmune disorder where your body attacks itself.
Crohn’s Disease
Symptoms related to inflammation of the GI tract:
• Persistent Diarrhea
• Rectal bleeding
• Urgent need to move bowels
• Abdominal cramps and pain
• Sensation of incomplete evacuation
• Constipation (can lead to bowel obstruction)
More severe symptoms:
• Fissures in the lining of the anus (tears)
• Fistulas (tunnel from one loop of intestine to another or connects the intestine to the: bladder, vagina or skin)
Ulcerative Colitis
Symptoms related to inflammation of the Colon:
• Bowel movements become looser and more urgent
• Persistent diarrhea accompanied by abdominal pain and blood in the stool
• Stool is generally bloody
• Crampy abdominal pain
General symptoms that may also be associated with IBD:
• Fever
• Loss of appetite
• Weight Loss
• Fatigue
• Night sweats
• Loss of normal menstrual cycle
Types of Crohn’s Disease:
• Ileocolitis: The most common form of Crohn’s, ileocolitis affects the end of the small intestine (the ileum) and the large intestine (the colon). Symptoms include diarrhea and cramping or pain in the right lower part or middle of the abdomen. This type is often accompanied by significant weight loss.
• Ileitis: This type affects only the ileum. Symptoms are the same as ileocolitis. In severe cases, complications may include fistulas or inflammatory abscess in right lower quadrant of abdomen.
• Gastroduodenal Crohn’s disease: This type affects the stomach and the beginning of the small intestine (the duodenum). Symptoms include loss of appetite, weight loss, nausea, and vomiting.
• Jejunoileitis: This type is characterized by patchy areas of inflammation in the upper half of the small intestine (the jejunum). Symptoms include mild to intense abdominal pain and cramps following meals, as well as diarrhea. In severe cases or after prolonged periods, fistulas may form.
• Crohn’s (granulomatous) colitis: This type affects the colon only. Symptoms include diarrhea, rectal bleeding, and disease around the anus (abscess, fistulas, ulcers). Skin lesions and joint pains are more common in this form of Crohn’s than in others.
Types of Ulcerative Colitis:
• Ulcerative Proctitis: For approximately 30% of all patients with ulcerative colitis, the illness begins as ulcerative proctitis. In this form of the disease, bowel inflammation is limited to the rectum. Because of its limited extent (usually less than the six inches of the rectum), ulcerative proctitis tends to be a milder form of ulcerative colitis. It is associated with fewer complications and offers a better outlook than more widespread disease.
• Proctosigmoiditis: Colitis affecting the rectum and the sigmoid colon, the lower segment of colon located right above the rectum. Symptoms include bloody diarrhea, cramps, and a constant feeling of the need to pass stool, known as tenesmus. Moderate pain on the lower left side of the abdomen may occur in active disease.
• Left-sided Colitis: Continuous inflammation that begins at the rectum and extends as far as a bend in the colon near the spleen called the splenic flexure. Symptoms include loss of appetite, weight loss, diarrhea, severe pain on the left side of the abdomen, and bleeding.
• Pan-ulcerative (total) Colitis: Affects the entire colon. Symptoms include diarrhea, severe abdominal pain, cramps, and extensive weight loss. Potentially serious complications include massive bleeding and acute dilation of the colon (toxic megacolon), which may lead to an opening in the bowel wall. Serious complications may require surgery.
Causes and who’s affected:
As many as 700,000 Americans may be affected by Crohn’s Disease and Ulcerative Colitis. It is equally common in men and women and while it can affect a person at any age there is a higher risk during the years from 18-35. The cause of IBD is not fully understood but there is a connection between diet and stress; as well as hereditary, genetics and/or environmental factors that play a role in the development of IBD. Studies have shown a greater risk of 5-20% increase in someone acquiring this disease if a “first-degree” relative (parent, child, sibling) has it and an even greater chance if both parents have an IBD. Crohn’s is most common among people with Eastern European backgrounds and it is increasing in number for African Americans. Ulcerative Colitis is more common among Europeans with a Jewish background heritage.
The environment that you put yourself in plays an important role as well. The occurrence is higher in “developed” countries than in “underdeveloped countries, higher in urban areas rather than rural, and in northern versus southern climates.
Treatment with Chinese Medicine:
 Due to the differential diagnosis that is applied in Chinese Medicine there are different “patterns” that exist when dealing with a disease. This is a similar idea to the different types of Crohn’s Disease and Ulcerative Colitis described above. However, with Chinese Medicine, the patterns are based off of the symptoms the patient is currently experiencing as well as their history, their facial color, body odor, general demeanor, abdominal diagnostic, pulse diagnostic and tongue diagnostic. All of this information is compiled which leads to one of many “diagnostic patterns” to which the according acupuncture points, herbal formula, diet and lifestyle is prescribed. Chinese Medicine is a powerful therapy that can help treat severe cases and help keep mild cases and patients who are in remission stay in remission.
Due to the differential diagnosis that is applied in Chinese Medicine there are different “patterns” that exist when dealing with a disease. This is a similar idea to the different types of Crohn’s Disease and Ulcerative Colitis described above. However, with Chinese Medicine, the patterns are based off of the symptoms the patient is currently experiencing as well as their history, their facial color, body odor, general demeanor, abdominal diagnostic, pulse diagnostic and tongue diagnostic. All of this information is compiled which leads to one of many “diagnostic patterns” to which the according acupuncture points, herbal formula, diet and lifestyle is prescribed. Chinese Medicine is a powerful therapy that can help treat severe cases and help keep mild cases and patients who are in remission stay in remission.
Before we discuss the differential diagnosis, there are a few terms that need to be explained. First one is the “Organ” system. In Chinese Medicine each organ is attributed to specific functions that don’t necessarily match a scientific viewpoint. For example the “Spleen” and “Stomach” are considered to be in charge of the digestive functions and water metabolism in Chinese Medicine. The “Spleen” actually handles some of the function of the “Western” spleen, pancreas and small intestine. The “Liver” has to do with the free flow of qi, which is easily obstructed by stress, emotions, diet and lifestyle. The “Kidney” can be attributed to water metabolism, as well as genetics and our “reserves.” The term “burning the candle at both ends” is a great way to describe how stress and lifestyle can damage the Kidneys. The “Heart” has to do with our emotions and deals with blood. When the digestive system isn’t absorbing food properly we cannot produce the nutrients and blood needed to support these organs. “Heat” refers to inflammation and “Dampness” refers to water metabolism malfunction. Both of these can manifest in numerous ways, as you will see below.
Below are examples of some different patterns that could be “diagnosed” as Crohn’s Disease or Ulcerative Colitis and what the treatment principle should be.
• Spleen Qi Deficiency: Intermittent dull abdominal pain that is alleviated with pressure, abdominal distention, early satiety, nausea, loose stools or diarrhea, loss of appetite, waxy pale or sallow complexion, fatigue, weakness, shortness of breath with exertion, spontaneous sweating, dizziness, and light headedness. Might have mild bleeding of dark, purplish blood, or less commonly, red blood preceding or following a bowel movement; or black, tarry, sticky, unformed stools; or occult blood in the stool discovered upon routine testing. There may be other signs of bleeding, such as heavy menstrual periods or easy bruising.
- Tongue: pale and swollen, with tooth marks (or pale and thin with significant blood deficiency).
- Pulse: Thready and weak or moderate.
- Treatment Principle: Strengthen Spleen, supplement and elevate qi. Nourish Blood and stop bleeding.
• Liver Qi invading the Spleen: Recurrent Diarrhea which may be urgent and preceded by cramping abdominal pain. The pain is relieved following defecation. The diarrhea may alternate with constipation. Symptoms become worse with stress and tension or eating. There is a possibility of mucus and blood in the stool. Other signs and symptoms include abdominal distention, poor appetite, nausea, heartburn, indigestion, borborygmus, flatulence and belching, which relieve abdominal discomfort, hypochondriac discomfort, ache and tightness generally worse on the right side, irritability, depression, moodiness, shoulder and neck tension, temporal or tension headaches, cold fingers and toes, premenstrual syndrome and breast tenderness.
- Tongue: normal or darkish body, or pale, or with slightly red edges: greasy coat especially over the root (depending on the degree of heat, deficiency and Dampness.
- Pulse: Wiry
- Treatment Principle: Harmonize the Liver and Spleen, regulate Liver qi, Support and strengthen Spleen, Alleviate spasm and pain, and stop diarrhea.
• Blood Stagnation: Chronic Diarrhea with a feeling of incomplete evacuation or tenesmus. The stools may be purple or black, sticky or tarry. The diarrhea may alternate with constipation.Fixed and localized, sharp or stabbing abdominal pain (usually in the lower left quadrant) which is worse with pressure. Dark complexion, dark rings around the eyes and purple nails. Spider naevi or vascular abnormalities over the abdomen, face and legs (particularly the inner knee and ankle).
- Tongue: purple or with brown or purple stasis spots; sublingual veins dark and distended
- Pulse: wiry, choppy or thready.
- Treatment Principle: Transform and eliminate stagnant Blood from the Intestines.
• Damp Heat dysenteric disorder: Frequent, foul smelling, explosive diarrhea with blood, mucus and pus: the mixture of mucus and blood will vary depending on the balance of Heat and Damp.Burning anus, tenesmus, colicky abdominal pain, abdominal distention, scanty concentrated urine, red complexion, red eyes, dry mouth, and thirst (maybe with little desire to drink). In the early stages there may be fever and chills, headache and a floating pulse.
- Tongue: greasy yellow coat; with more Heat a red tongue body and a dry coat; with more Dampness, a thick greasy tongue coat
- Pulse: slippery and rapid.
- Treatment Principle: Clear Damp Heat from the Intestines and Regulate Qi and Blood, stop pain.
• Spleen and Kidney Yang Deficiency: Chronic and relentless diarrhea which is thin, watery and mucoid, and may contain pus and blood. In severe cases there may be incontinence of stools and rectal prolapse. The diarrhea is worse from exposure to cold and cold foods. Mild tenesmus or a dragging sensation in the lower abdomen, not relieved by diarrhea. Mild persistent abdominal pain, which is better with warmth and pressure. Loss of appetite, listlessness, fatigue exhaustion, depression. A waxy pale or sallow complexion, cold extremities, cold intolerance, weakness and soreness of the lower back and legs.
- Tongue: Pale and swollen with a thin white coat.
- Pulse: deep, thready, weak and slow.
- Treatment Principle: Warm and Strengthen the Spleen and Kidney Yang. Disperse Cold, transform Dampness. Astringe diarrhea and elevate qi.
• Yin Deficiency with Residual Damp Heat : Chronic diarrhea with small quantities of sticky mucus and blood. Frequent urge to defecate but often in vain. Mild lower abdominal pain, tenesmus, loss of appetite, nausea, dry mouth and lips, thirst worse at night, afternoon or tidal fever that’s worse at night. Heat in the palms and soles, nightsweats, flushing , emaciation, weight loss.
- Tongue: red or scarlet and dry, with a greasy or peeled coat.
- Pulse: thready and rapid.
- Treatment Principle: Nourish and supplement yin and clear residual Damp Heat. Nourish and regulate Blood and stop dysentery.
• Heart and Kidney Yin Deficiency: Recurrent mouth ulcers, which appear in clusters and tend to aggregate on the tongue or tongue tip. The ulcers are painful and hot, with a narrow, slightly swollen, mildly red margin. They frequently recur and persist for up to several weeks before resolving. Often of many years duration, the ulcers tend to be provoked or aggravated when the patient is stressed, anxious or upset. Nervous, anxious individual, insomnia, vivid dreaming, panic attacks, palpitations, forgetfulness, dizziness, tinnitus, lumbar ache, sensation of heat in the palms and soles, dry mouth and throat, night sweats.
- Tongue: red with little or no coat, redder at the tip.
- Pulse: Thready and rapid.
- Treatment Principles: Nourish Heart and Kidney yin. Clear Heat, calm the (spiritual) Shen.
Forms of treatment include acupuncture, herbal formulas (which can be taken internal or external), Massage/tuina, dietary therapy, exercise and lifestyle consultation. When we utilize and multiple forms of therapy results are seen at a rapid rate.
*Disclaimer: The information offered in this paper is not intended to diagnose but rather to inform the public about IBD and give a brief look at how Chinese Medicine looks at and treats IBD.
References:
• http://www.ccfa.org /
• Will Maclean and Jane Lyttleton, (2003), Clinical Handbook of Internal Medicine “The
Treatment Of Disease with Traditional Chinese Medicine” Volume 2 Spleen and Stomach, University of Western Sydney