Having returned from Mayo, I want to post a quick update…. I’m good, under the circumstances—not going to let having this disease change things too much. I saw my GI at Dartmouth yesterday. He was surprised I went to the Mayo Clinic, but understands how seriously I consider taking DNA-altering drugs, and drugs that affect my immune system, etc. His colleague, Corey Siegel, is doing a study of using a different kind of Tumor Necrosis Factor (Alpha) inhibitor (big fancy words I am loving to say, but suffice it to say it is human and not mouse-tissue based); the results of which will be available in a few weeks. They want me to wait since I have no symptoms, and waiting is what I do best!
Dr. Bensen said if I take the drugs, they are seeing the best results with the TNF(A) Biologic (he mentioned Humira) (also Remicade and Cimzia), combined WITH the immunomodulator, 6MP, for the best results for full remission, at 40-60%. He said if I take the Imuran alone, my chances of getting results are not as efficacious. This, I do understand. He feels the Mayo Clinic’s recommendations are not fully in line with his, and Corey Siegel’s, “front-line” offense approach.
~
In the meantime, I am (seriously!) looking into taking whipworms….you know how much I love creepy crawly things! Seriously, there is a new study, and you can read about it here.
It is nice to be back home in Vermont…. The day I left Rochester, Minnesota, there was a blizzard and they got around 13 inches of snow in MAY!
I am working on a longer post about the stress reduction class I tool, the Eastern medicine and work of Amit Sood, MD, and the integrative medicine at the Mayo Clinic.
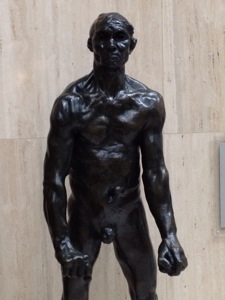
Here are a few more photos from Mayo (top, Fish, by Gordon Gund a patient; bottom statue study for the “Les Bourgeois de Calais,” by Aguste Rodin…a huge statue that is very powerful and stands in the middle of a busy atrium cafeteria looking anguished; and last but not least, the dancers I really fell in love with in the hallway near the blood work laboratories!)…
waiting for the doctor
April 30 Tuesday 4:30 PM
I am waiting for Dr. Jeffrey McCurdy and he will review my case with me.
Monday I had a CAT scan here at the Mayo Clinic. I had not eaten for 24 hours, due to the requirement to be fasting for my appointments. I think because of that, I ended up fainting.
I could tell I was feeling a little sick, and the staff was incredible — they were so wonderful. Anyway, I was wheeled into the CAT scan room, and my technician James even joked with me about me fainting (word had spread!).
They are all incredibly nice here at the Mayo Clinic. The buildings and the grounds are really quite spectacular. It reminds me of an unknown Mecca of sorts, or a place where people go to pilgrimage. It is interesting that my son, Sam, is on a pilgrimage called El Camino de Santiago, in Spain, at this time. There are so many people here, from all over the world—many of whom are very sick, or caring for a loved one who is sick—and there is a sense of the fragility of life around me here, but also the indomitable spirit of the patients in search of extending their lives or, as in my case, improving the quality of life.
So, while I’m waiting for Dr. McCurdy, I am prepared to take in the news that they will recommend that I take medication. On the other hand, they may suggest some alternatives. I have no idea!
After the affable, and highly intelligent 30-something, Jeffrey McCurdy, MD, arrived he sat down and showed me my blood work results (spectacular were his words!), and my CAT scan results (not so great, in his words), the medication, IMURAN, is recommended by the GI team here at the Mayo.
My Tpmp is normal, so they say I can take the maximum dosage. (Thiopurines are a class of drugs that suppress the immune system. Examples include azathioprine, mercaptopurine, and thioguanine. These medications are used to treat diseases such as acute lymphoblastic leukemia, inflammatory bowel disease, and autoimmune disorders. They may also be prescribed to patients who have had organ transplants to help delay or prevent organ rejection. This test detects the activity level of the enzyme thiopurine S-methyltransferase (TPMT) in a person’s red blood cells. The activity level of TPMT is associated with the ability to effectively metabolize thiopurines.)
Dr. McCurdy explained that I have a high “Rutgeerts” score of 3 on my colonoscopy, which is indicative of inflammation that they usually treat aggressively.
Blood work checks will be frequent to monitor my side effects. Uncommon side effects are rare, but can be severe. Flu-like symptoms (most common), headaches, joint pain can be severe, fevers, pancreatitis, elevated liver enzymes (blood work will be checked for this). There is also a possibility of a decrease in my white blood cell count, which helps you fight infection. They expect it will go down… Mine is currently at 6.4 Leukocytes (might go down as low as 3.0).
Very uncommon risks are as follows: Cancer risk for skin cancer, so skin exams yearly are recommended. Also, there is an slight increase in the possibility of lymphoma—When I asked him to explain, he provided an analogy of a busy street corner, with 2 out 10,000 passersby might have lymphoma. With IMURAN, this chance increases to 4 in 10,000.
Of more concern is the inflammation in my body. I can develop perforations, strictures, flistulas, and abscesses due to bowel perforations. Having active inflammations increases my risk of cancer, which is exceedingly uncommon in the small bowel, but worth noting. If Dr. McCurdy were in my shoes, he said he’d do both medications at once: Remicade and IMURAN. But, he also spent hours reviewing my case with Dr. Tremaine, and since I’ve been 7 years out of surgery, I have a better argument for not taking the two types of medications recommended by Dr. Corey Siegel at Dartmouth. In 2010, my histogic (tissue) endoscopic test was minimal, showing only 4 ulcers, scoring a “Rutgeerts” score of 1.
For me to decide medications, it is highly individualized, and they know I’m in line with alternative medicine. Given my individual history and predications, they recommend a one year duration with a colonoscopy to show results. (I.e., one year before investigations.) using the maximum dose of Imuran.
Right now, I would need to be on it indefinitely. When medication is stopped, the disease tends to comes back, and some people may no longer respond to that medication should they go off and develop a recurrence.
In Crohn’s disease, they know that for causes genetics is involved, and environmental factors. However, there is no known cause or cure. Parasites activate a certain arm of your immune disease, but it is very unlikely it would cause a disease such as Crohn’s. No single organism is ID’d as a causative agent. Fecal transplants and worm therapies are being studied. Only case studies available: meaning when studies are positive, they are quick to publish, so there is sometimes a publication bias. It is important to report positive-negative outcomes to determine efficacy. He said he worries about safety with introducing pathogens (like worms!); and they need more information on safety profiles.
The SCD diet (specific carbohydrate diet): science on this is not conclusive, according to Dr. McCurdy, and diet depends on state of bowel disease.
They know that for many patients animal fats, simple sugars, and shellfish can contribute to the disease. My disease is characterized by inflammation.
Dr. McCurdy has little experience with herbal remedies. He said to be careful with anti- inflammatories like Advil and Ibuprofen, because they can make Crohn’s worse.
Lots of his patients use Vitamin D (in patients that are deficient), with good results, but not using therapeutically, though there are recent studies on vitamin D and Crohn’s specifically.
If I wait, I’m running risk of developing strictures, flistulas, and a possible bowel obstruction. I already had an internal fistula in 2006, but I could develop cutaneous (out of skin), or vaginal, fistulas, or other connections from one organ to another, which are symptomatic of Crohn’s. again, he noted that I am symptom free, except for the endoscopic and CAT scan tests.
Dr. McCurdy just did a presentation on new therapies that use different mechanisms of action in clinical trials. These are years out, he said.
I have swollen lymph nodes around my disease site: any time you have inflammation, your immune system starts in the lymph nodes, like in a common cold when your lymph nodes swell. I have inflammation around 10 cm of the neo- terminal ileum.
They don’t want me to loose anymore small bowel because of problems with malabsorption, especially Vitamins and minerals.
So, that’s the report…I guess I was hoping that my CAT scan would have been better. It is really hard to live with a disease and not see improvements.
My next stop is the Integrative medicine round, and I will explore a lot of alternatives—for sure!
Stay tuned for Day 3, where I visit the Stress Reduction & Relaxation Clinic at the Mayo…
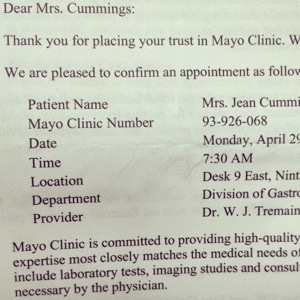
I am waiting for Dr. Jeffrey McCurdy at the Mayo Clinic — I will see him this morning April 29 at 8 AM.
I arrived last night at 6:00 pm at my hotel the Kahler Grand in Rochester Minnesota, having departed from Hartford airport in the afternoon. The flight was an easy three hour flight. The people here are extremely friendly so far.
I am not nervous, in fact I feel very confident. When I got here I was very impressed by the architecture and the huge buildings of the Mayo Clinic. Everything is so beautiful here: the artwork on the walls and the whole ambience of the place.
Dr. McCurdy was great. He’s from Canada. He is in his early 30s. He asked me tones of questions about the history of my disease. He was very thorough, and I got a complete physical exam.
My weight was 138, my blood pressure was normal, and my first rectal examination was normal. Around 40% of Crohn’s patients have some sort of anal-rectal problem. Things like fistulas or discharge. Luckily, for me, I do not have any problems there.
Enterography Is a possible test they might perform, according to Dr. McCurdy.
A new study from Rhode Island Hospital has found that MR enterography (MRE) without the use of an anti-peristaltic agent was as reliable as CT enterography (CTE, or CAT scan) in determining the presence of Crohn’s disease “without the use of an anti-peristaltic agent.”
In other words, this test exposure to ionizing radiation is less invasive, especially for children who are prone to absorbing more radiation than someone in their 50s like me!
Disease reccurrance after Crohn’s surgery is the rule, according to my doctor, at around 90%, and it comes back in 2-3 years. Patients can be asymptomatic but have disease.
I have gone 7 years!
Dr. McCurdy noted that “treating for mucosal healing is the best chance I have without complications.”
He also gave me my options and course of testing:
“So there are number of predictors that we have determining who’s going to have a more aggressive disease course: clinical predictors, imaging predictors. as well as other diagnostic tools.”
In the clinical predictors, he said, there are patients who have had several resections who have symptoms that come back immediately after the resection as well as people who don’t have any symptoms.
Endoscopic predictors (colonoscopies) are the best predictors of who will have no complications in the future.
In 2008, a Belgian clinician, Paul Rutgeerts, MD, developed an endoscopic score to predict who will develop problems in the future and it’s based on how much inflammation is found in the scope. So a Rutgeerts scored of 0 means zero inflammation; a Rutgers score of 1, which is what I had in 2010, showed some inflammation.
More than 5 ulcers and confluent inflammations — that would be a Rutgeerts score of 3 — that’s what I have now….A Rutgers score of 3 or 4: that’s when you start to get worried about future complications. Since I have a Rutgeerts score of 3, that predicts — with about 75% predictive value— that I will develop problems with Crohn’s disease in the future.
“So that’s what we have to go by,” he said, “and when you’re working with medications, you only think about people that need medications, and we also think about those clinical predictors, as well as disease recurrence in some patients that require surgery.”
If patients score less on the Rutgeerts scale, and they have a lower risk profile, they don’t need any medications; and in these patients that don’t take any medications, they scope from 6 to 12 months after surgery and look for that Rutgeerts score, which is what they’ve been doing with me up at Dartmouth.
I have no symptoms, but Dr.McCurdy said I have significant disease at this time, which is predictive of problems down the road.
The question they have now is how long has this disease been spreading, and how extensive it is.
The more extensive it is, the more aggressive they are with medications —if it’s a very small segment, then it is very reasonable to consider surgery, if I want, but the risk of surgical adhesions is high.
Dr. McCurdy will determine how long that segment is by doing what what’s called CT enterography which is a special scan to look at the small bowel.
“Okay, so what we should do this,” I added.
He said we should also get my biopsies from November, to look at the pathology slides to make sure that they confirm that this is Crohn’s disease and nothing else.
He added, “then I always do a routine blood test to check vitamin D levels and B12 levels, as that’s the area that’s been removed called the terminal ileum (he pronounced it with a long “I” sound and when I asked him, he said he is the only doctor who pronounces it “eye-leum”).
He added that whether we should be using medications, or whether we recommend surgery or no medications at all, will need to be determined…
“At the end of the day,” he added, “we will recommend what we think is best for you, and then you’re the one who ultimately makes a decision on what you do based on your values and what you think.”
He said, “I will give you several options what I think is the best approach based on the current literature and then you can make a decision on what you think sounds okay.”
More to come!
¡Hola! My fellow Crohnies, uc-ers, readers . . . My friend, Shelly, asked me what was up, so I thought I better get on here, and write something! Having Crohn’s disease AND colitis, and other autoimmune diseases is not a walk in the park, but my girlfriend, Cindy, has something called myasthenia gravis, and she is really struggling. Last night, I had a home jewelry party as a way for her to raise money to help defray some medical expenses, and the upcoming mortgage (she ‘s a single mother of three on disability). It felt great to help HER! I think helping others is the way to help ourselves….
So now, the update!
Crohn’s flare Novemeber 30th Rx.
Started low dose naltrexone, high potency turmeric, increased probiotics, and something called Glutamine (the last 2 on an empty stomach), along with high potency turmeric (cur-cumin—yes, an herb!). I told my GI I was doing this…. And now it is over two months later, and I feel great!!! This is definitely NOT a drug or infusion with potential side effects (though LDN is not FDA approved), rather it is a more “integrative” approach to medicine that should be practiced everywhere. I’m lucky, in that my co-author, Jessica Black, is a naturopath who is up to date on treatments that are less invasive, but effective! Worth looking into, don’t you think?!
After I started writing this post, I looked up Glutamine, and this is how it works:
With the anti-inflammatory, Cur-Cumin, and the beneficial effects of increased probiotics, the Glutamine works as a binder in my gut to help decrease the inflammatory cytokines. It is an amino acid. The probiotics are live culture micro-organisms that help to balance the gut micro flora. This is good stuff! The doctors, the researchers, and patients are beginning to take all of this gut bacteria science news pretty seriously.
Onward!
“The human gut teems with bacteria, many of their species still unknown. They help,us digest food and absorb nutrients, and they play a part in protecting our intestinal walls. Gut bacteria may also help regulate weight and ward off autoimmune disease.”
I strongly feel that taking a regimen of potentially carcinogenic drugs is not the way I, personally, want to go! I HAVE taken Prednisone, and currently I am on a low dose (3mg) naltrexone protocol (this is NOT FDA-approved), and I just know it is working.
A feeling of consistency is occurring—getting at least 8 house of sleep, walking-running 3/4 miles a day, doing yoga and meditation daily, seeing a therapist…. And writing about it all. This kind of integrative medicine is where we should all head towards, as patients and caregivers!
~
Here is the coolest photo in the world…. Can you guess what it is a photo of???
From National Geographic!
“What goes around comes around . . .” may actually be an old proverb meaning “the status eventually returns to its original value after completing some sort of cycle”. . . . Or, “a person’s actions, whether good or bad, will often have consequences for that person.”
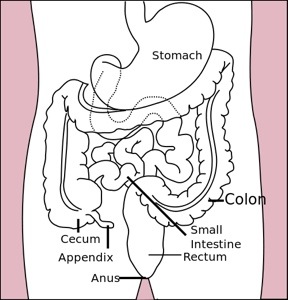
I am thinking about that old saying a lot lately, due to the news that I have a severe recurrence of Crohn’s disease. Crohn’s can be found anywhere in the intestinal tract, from the mouth to the anus, but it usually presents in the terminal ileum, as it did in my case. Since I no longer have the 20 centimeters of terminal ileum (or the ileo secel valve that links it to the large colon), I now have the spread of the disease on the other side of my sutchers…. 20 more centimeters of small bowel are severely inflamed. For the record, that is a total of almost 2 feet, 20cm being around 8 inches. Here is a good definition:
The small intestine (or small bowel) is the part of the gastrointestinal tract following the stomach and followed by the large intestine, and is where much of the digestion and absorption of food takes place. The primary function of the small intestine is the absorption of nutrients and minerals found in food. The average length of the small intestine in an adult human male is 6.9 m (22 feet 6 inches), and in the adult female 7.1 m (23 feet 4 inches). It can vary greatly, from as short as 4.6 m (15 feet) to as long as 9.8 m (32 feet).[3][4] It is approximately 2.5–3 cm in diameter. The small intestine is divided into three structural parts: Duodenum, Jejunum, and Ileum.
The small intestine is where most chemical digestion takes place. Protein, lipids (fats) and carbohydrates are broken down and a process called diffusion takes place where nutrients are absorbed into the blood vessels through the wall of the small intestine (the terminal ileum is where the B-12 and bile salts are specifically absorbed). There are all sorts of mucosa and wrinkly tissue down there—hence the language from my latest colonoscopy had terms like “serpentine” to describe the tracks of inflammation they found). There is a lot going on in the bowel—the second brain—including the delicate villi, which is Latin for shaggy hair (I love these descriptions!).
Do you have Crohn’s or uc?
If so, we have even more in common! Interestingly, I keep my book off my Facebook personal page—not to hide my disease, but to not “promote” my book, for fear people will think I am only selling a medical memoir written with a naturopathic doctor to make money (not!!).
Maybe I should become brave like Mike McCready, and be even more open….in this teeny tiny post, I will explain that I have lived with this sucky disease since I was in college, and was only diagnosed when I was forty.
When I turned 50, I lost a significant portion of both large and small bowel, and I have enjoyed a great quality of life ever since my surgery—pain-free! What a joy to have my life back!!! I take nothing for granted, and I wake up each and every day feeling blessed and lucky (I’m Irish), and I do not like to listen to self-absorbed people talk on and on about, you know….. Anyway, as I was sayin’ …. My book is ranked number 11 on Amazon in disease, and consistently No. 1, 2, or 3, in Kindle’s Gastroenterology ranking. Many people actually write to me and say thanks—the greatest gift in the world! I want to say “thank you” to my readers, my friends, and all of the community—anyone who has struggled with disease, or losing a loved one—we are all connected!
What does Karma mean?
A Sanskrit word, and one from Hindu-Buddhist religious traditions, it means that “the total effect of a person’s actions and conduct during the successive phases of his existence, regarded as determining his next incarnation.” I don’t know about you, Dear Reader, but I am ready for this cycle of disease to be over!
From the Dalai Lama
Take into account that great love and great achievements involve great risk.
When you lose, don’t lose the lesson.
Follow the three R’s:
– Respect for self,
– Respect for others and
– Responsibility for all your actions.
Remember that not getting what you want is sometimes a wonderful stroke of luck.
Learn the rules so you know how to break them properly.
Don’t let a little dispute injure a great relationship.
When you realize you’ve made a mistake, take immediate steps to correct it.
Spend some time alone every day.
Open your arms to change, but don’t let go of your values.
Remember that silence is sometimes the best answer.
Live a good, honorable life. Then when you get older and
think back, you’ll be able to enjoy it a second time.
A loving atmosphere in your home is the foundation for your life.
In disagreements with loved ones, deal only with the current situation. Don’t bring up the past.
Share your knowledge. It is a way to achieve immortality.
Be gentle with the earth.
Once a year, go someplace you’ve never been before.
Remember that the best relationship is one in which your love for each other exceeds your need for each other.
Judge your success by what you had to give up in order to get it.
If you want others to be happy, practice compassion.
If you want to be happy, practice compassion.
Seems like my own health has taken a bit of a dive ;( … when I was freaking out about Lyme disease, it turns out it was a Crohn’s flare-up. Yes, I have been so happy to be in clinical remission for the past 6-1/2 years, I’d forgotten what it was like to have a flare up!
I thought I had Lyme disease, and was having stiffness and flu-like symptoms. Some of my readers will remember that I had a systemic flare of poison ivy during the first half of the summer (yeah, five weeks on Prednisone was not fun;( … Well, my dermatologist thinks the acute contact dermatitis (poison ivy resin is powerful stuff, not easily washed off and stays on your work gloves I learned!) caused my body to get out of balance, and I think she may be right! There is a strong connection between the skin and the gut — more on that subject in a later blog post.
I was at Dartmouth Hitchcock this week for a colonoscopy, and my results were very discouraging. My small intestine is in an active flare, characterized as severe. The news could have been better that is for sure! I am still in shock. My small intestine is riddled with Crohn’s in a 20 centimeter area just near the former surgery. Crohn’s is incurable and when it does this, they get serious and make you take these auto-immune suppression drugs. The recommended drug, 6-MP, is an immunomodulator – the way it works is it suppresses your immune system so that your own immune cells will stop attacking the lining of your intestines. There are patients who tolerate the drugs and it helps them stay in remission and pain free. Others have reactions to the drug, like fevers and stiffness. What the doctors look for at the beginning is liver damage.
On Thursday, after my colonoscopy, they got me right to the lab to draw blood for the test to determine if I could tolerate the 6MP. I, of course, started talking to my wonderful GI, Steve Bensen, about not taking the drugs. Couldn’t I work with my naturopath, I reasoned, and take the less toxic drugs she prescribes, and come back in 3 months for a scope? I did just finish a heavy round of Doxy for the symptoms of Lyme disease (for the record, I had an engorged deer tick that I pulled off and squashed and flushed down the toilet — always save the tick to be tested!), so the antibiotic had upset my stomach.
The head of the IBD Clinic, Cory Seagel, even came into my little curtained room with me in my Johnny gown sitting on the side of the bed. “You should start the drug immediately if your liver can tolerate it, better yet, you should take a combination of 6MP and Remicade,” he said.
Here is a good definition from Livestrong:
6-Mercaptopurine, or 6-MP, is a purine analogue antimetabolite drug that is used in the treatment of acute lymphoblastic leukemia, Crohn’s disease and ulcerative colitis. Purine analogues impair DNA synthesis, leading to less cells being created. Acute lymphoblastic leukemia, Crohn’s disease and ulcerative colitis are all conditions of an overactive immune system. 6-MP helps to decrease the amount of immune cells in the body to help control the disease.
The findings
The colon appeared normal. My sigmoid resection at 15 cm and its short blind colonic pouch had normal anastomosis (a term for surgical connection)….This is good news! Large intestine: check.
Ileal resection: segmental inflammation characterized by erosions, erythema, fir ability, granularity, loss of vascularity, confluent deep ulcerations, and serpentine and shallow ulcerations found in neo-terminal ileum and extended from my first surgery for 20 cm (about 8 inches)…. Small intestine: NSG (not so good!)
The power of poetry/intention
There is something about the language of medicine that I find vaguely hypnotic and poetic. Weird as it sounds, understanding the human side of medicine is an intention of mine, and one that I hope to impart on my readers, should they desire to learn more!
The path ahead
I wish I didn’t have this new problem, and feel fine! I went 5-10 years last time, but this time the wall of the small intestine is compromised and thinning. I may be flying out to the Mayo Clinic, for a second opinion and work-up involving their more integrative approach. I am a wreck about this, of course, but trying to stay focused. As my daughter, Emma said, I have such resolve and a positive attitude… Don’t feel like dwelling on it too much, but wanted to let my (our) wonderful readers know why I’ve been out of touch. I am going to start with the naturopathic doctor on Tuesday….. and Mayo Clinic, probably in January.
Notes from Jessie Black, ND
Let’s work with an accompanying pharmacist and try low dose naltrexone — start very low and amp up to 4.5 milligrams. In addition, she mentioned a very powerful high-potency coated turmeric (this is hard to absorb, so it’s necessary to work with a naturopath who knows their herbal medicine), and a new, more fiscous fiber called PGX. Fiber is something I take daily, already, along with garlic, Aloe Vera, extra C, D vitamins, calcium and multi-vitamins and Omega 3 capsules. A good article about helpful herbs is found here

Dede in the recording studio at VPR. I am happy when I am writing!
My basic diet now: No caffeine, dairy, processed foods, alcohol and trans fat. Instead SCD-certified food, lots of fresh-steamed veggies, cold water fish, and other foods from SCD! An awesome site for basic dietary help is found here! Link to a flare-up diet.
This blog will detail my journey. Thanks for your support and being part of it all! I welcome comments and suggestions, especially from IBD sufferers who have taken other meds besides 6MP and Remicade. Or IBD patients who have taken the drugs and had good results…I want to examine and research both options, along with a more integrative approach to possibly even healing the current severe inflammation without drugs!
I will start off by following my co-author and naturopath, Jessica Black’s Anti-Inflammation Plan (diet and lifestyle) that is in our very own book, Living With Crohns & Colitis!
- caffeinated beverages
- fried foods
- processed foods
- peanut butter
- carbonated soda
- citrus
- wheat
- pork
- tomatoes
- potatoes
- dairy
- sugar
- eggs
- shellfish
- peanuts
- anything that contains hydrogenated oil
After four weeks, reintroduce the eliminated items, one per week and if no allergic symptoms occur, add the item back into the diet. Read more More to come….
Blessings, Dede
Oh, dear: it is that time of year again . . . Time to schedule my annual colonoscopy, or “colo,” as my gastroenterologist, Dr. Steve Bensen refers to it, in the casual, behind-the-scenes way he talks to his fellows and medical interns, nurses and doctors. Since my book came out, and I presented him with a signed copy just two years ago, our bond has thickened, and luckily my small intestine has not (pun intended!).
Bensen has been my GI doctor ever since the doctor at the big-city teaching hospital I will not name (Boston area), told me to take 6MP, or if I persisted in my quest for a combination of naturopathic remedies and Western medicine, to “eat squishy food!” The fact that this eminent Harvard-trained department head would tell me to “eat squishy food” struck me as hilarious at the time, but it turns out he was entirely correct, in that my disease is characterized by scarring and narrowing of the small intestine due to flare-ups, and eating squishy food is actually great advice!
Having medical tests is physically, and often emotionally, draining. For example: Why would I go all the way to Boston, from my home on a dirt road in rural Vermont, deal with traffic, parking, and stress, wait at the X-ray department for one hour after swallowing tons of vile-tasting barium, only to be told by the X-ray technician that he was “going to lunch?” . . . I have lots of stories!
Ergo, my switch to the compassionate, smart, jovial, encouraging doctor, Steve Bensen, I have now. When I searched for a specialist, I went immediately to the ccfa.org website where they say:
Find a Healthcare Professional
Whether you’re trying to find a Crohn’s doctor or an ulcerative colitis doctor, trying to locate an experienced surgeon in your region, or searching for a dietician, you’ll probably find them in our listings. Search for providers by name or by the state and ZIP code in which they practice, as well as by specialty. Our list consists of leading Crohn’s and ulcerative colitis doctors, researchers, nurses and other healthcare professionals working in the field who have chosen to become members of CCFA. We cannot make recommendations about specific physicians or guarantee that all members listed specialize in the treatment of Crohn’s disease or ulcerative colitis. CCFA cannot attest to the credentials of its members, nor do we evaluate the competency of our members.
I figured a doctor who was current on all the ccfa.org research, studies, and developments in the field would be a good doctor for me. I nicknamed him “the Nordic god” (sorry, I know I am sexist and trivializing not only a country I love, but making the doctor sound like a model, which he could be, and if this were a man writing about a woman doctor I would probably be offended!), and our doctor-patient relationship begin almost twelve years ago. His staff is great—they remember my nickname is “Dede” and the nurses always ask me what I am taking in terms of vitamins and supplements, and they offer Ayurvedic teas, especially my favorite called “Smooth Move” (I kid you not!).
I am lucky to have such a welcoming and supportive clinic, but that does not diminish the anxiety of calling to schedule your annual “colo.”
For me, as a surgical patient, my fears are justifiable: there is a 50-60% reoperation rate after ileal-secal resections, and that is plenty to worry about for those of us who are trying to lead healthy lives after suffering for years before surgery.
Okay, now to get to my point: I am lucky to have a great clinic, doctor, surgeon, etc., however the other day I called the Endoscopic scheduler “AS PER MY INSTRUCTIONS ON THE SHEET THEY MAILED ME (caps, mine for emphasis!), after much trepidation, anxiety and fear, delay, denial….. you get the picture. They put me on hold, and the man came back and said, “Sorry, we can’t schedule your colonoscopy because you are calling too soon for an October test.”
I took a deep breath, and realized how anxious I’d become. Obviously, it isn’t his fault, and it is just hospital bureaucracy’s fault. I thanked him for his time, and went to my basement yoga-meditation area (I like to call it my yoga “studio”) and when I got to the meditation, I felt the stress let go, literally, from the top of my head—my mind, and its medical worries contained therein, became an empty void, a clean slate, a tabula rasa, and in place of fear and anxiety, I felt trust and healing. I will call back and schedule that test in a month . . . To be continued!
~
I was interviewed by Marisa Cohen for her story in Prevention Magazine entitled Four Screening Tests Women Fear. In the article, under item #2 (COLONOSCOPY), I am quoted about prep for a colonoscopy and she mentions our book! Anything that empowers women, as well as other patients with IBD, to take care of their bodies and relieve the fear of invasive medical tests is a good thing! Happy to be part of such a great article.