It is amazing how much a positive attitude can help. In our book, there is a section when I am despairing and a doctor comes and sits with me and holds my hand—no kidding! He said, “Think positive.” Well, on that note, I want to write a post today about that and helping the body adjust to the changing season and of course living with IBD in general. I also want to share the news that I am writing a cookbook, called Living with Crohn’s & Colitis Cookbook (good title, too!)…my publisher is the wonderful Hatherleigh Press, which is distributed by Random House. I couldn’t ask for a better team! Publisher, Andrew Flach believed in this book from the very start, associate publisher, Ryan Tumanbing is always there when I need things, and my editor, Anna Krusinski is da Bomb!
My book with Jessie is a good overview and a way to understand how the body chemistry and immune response works. I am not denying the benefits of medication, but we do offer an alternative, and if you are someone who has to stay on meds, you can do both—no matter what, it is important to keep the body tuned and in a balanced state of homeostasis.
Getting a full work up from a medical professional is the first step—go to a specialist at a GI clinic (Dartmouth is the best in my area), and have a colonoscopy, blood work (really important as many patients are anemic due to blood loss, or low in B-12 as in my case), a physical exam (a patient will no doubt be embarrassed by this like I was, but this is a very important exam because the doctors can determine a lot when they examine the anus and rectum, and palpitate the abdomen—they could feel the mass in my case), and what is called enterography: a MRI or CAT scan (I don’t recommend CAT scans too frequently for younger people) will reveal areas of disease inflammation.
Crohn’s typically presents in the lower right abdominal quadrant (often confused with the appendix!) of the small intestine, but it can strike anywhere from the mouth to the anus. Colitis presents throughout the large intestine only. Crohn’s really cannot be cured, and has a tendency to skip to infect the next section of the bowel even after the diseased section has been removed (as in my case). Colitis can be cured through surgery if nothing else (drug therapy or naturopathic-holistic-alternative) works. They take out the large colon, and connect the stomach-duodenum-small bowel through a J-pouch internally, or an external ostomy bag. Not a great thing for anyone to have an ostomy bag; however I have met many people with colitis who don’t mind the bag at all, and love the fact that they are pain-free.
The Crohn’s & Colitis Foundation of America is the best organization! I love everyone there, and run in their half marathons with Team Challenge to help raise money for research; plus it is a community of fellow patients, young and old, and we are a surprisingly close-knit group. Join, and sign up for a walk and a support group (they even have a new college group!) as soon as you can.
The other thing to do, is have a poop sample tested (this is no fun, but can tell a lot—bacterial infections, or something called C-Diff). In addition to going to a GI clinic, make an appointment for a work-up with a recommended naturopath, a trained naturopathic physician with a four-year degree from a well-known college (Bastyr University, for example) and get right in there for a checkup and a plan of action. My naturopath did allergy testing to see if there were specific foods (most common culprits are wheat and dairy), that I needed to eliminate, and she ordered an endocrine hormone test to see if I may have had a hormone imbalance.
I also give a lot of credit to my acupuncturist who is trained in Chinese medicine, and I go once a month. It is all in our book, but make sure you stay on top of the disease and get regular check ups with your medical doctor to rule out any other complications. I had a dangerous abdominal fistula, that didn’t show up on the CAT scan and was attaching itself to another organ—sorry to bring in the drama, but IBD (Inflammatory Bowel Disease) can be life threatening. No question, it is vitally important to be proactive, especially as a parent.
My weight was so low, I was dangerously thin—ironic, because our society places such status on being thin! I am now a healthy 140 pounds, and I work hard every day to stay healthy. Once I get busy with work, and let things slide, I start to feel run down… I can tell right away! Being in tune with your body is very helpful—keeping a food and daily journal, getting some good private counseling, and doing stress reduction exercises (Tai Chi or yoga) daily is also a big part of managing the disease.
I think I have covered the basic tenets of my book with Dr. Jessie. Oh, one more thing, join the online groups— http://www.ihaveuc.com, and The Crohn’s Journey Foundation for starters, also Intense Intestines, Girls With Guts, the Crohn’s Forum, Healing Well, and others. We are a strong and awesome group—always there to support each other! Let’s face it, the doctors are so busy, they can’t spend and hour with each patient, and it is the patients themselves who are doing great research and offering support. If a doctor tells you stress or diet have nothing to do with IBD, find another doctor! Oh, and second opinions are a good plan as well.
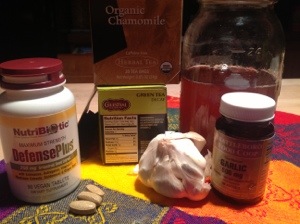
I have eliminated SUGAR, and ALL grains from my diet and ALL dairy. It is awesome! I feel so much better… I eat baked chicken or grilled fish, locally-raised, antibiotic-free, grass-fed hamburger steak once in a while when my body craves red meat, all served with yummy vegetables on the side and tons of fruit and nuts and eggs… I take extra calcium-magnesium, along with daily probiotics, turmeric, Omega 3, Vitamin D, herbal adrenal support, extra vitamin C, and a good multi-vitamin (I buy only organic food and supplements—it’s more expensive, but then I don’t spend a lot of money on clothes and makeup!).
So that is the basic overview—I am always there for my readers, and want to offer as much support as possible!
Oh, this just in, Dede will be on The Doctor Oz show this coming Monday, October 14th, in a spot on how common bloating is. They found me through the Crohn’s-Colitis book on “Help a Reporter Ou”t (HARO), and asked me to show how hard it is to buckle my jeans when I am bloated, which is what “used to happen” when I ate too much dairy or wheat…now, I don’t have bloating much AT ALL! Watch the segment if you want a laugh 😉 as “laughter is the best medicine.” I don’t mind embarrassing myself to help others…
Be well, and take care of yourself… don’t be afraid to ask for help!
Dede
Below, you can see some recent dinners… My husband and I have a grill we use a lot, and here you can see grilled marinated swordfish (fresh ginger root, white wine, wheat-free tamari, lime, and a dash of brown sugar for the marinade and let sit for a half hour before grilling) with grilled garden-fresh small eggplants (some people may have trouble with seeds…always introduce new foods slowly and note the reaction by your body in your journal right away….like I tried polenta this summer….noooooo! Not good for me, but may not bother someone else—we are all different!), and baked chicken with a sesame glaze (it was so good!) and steamed broccoli.
Greetings from Vermont. I am the co-author of Living With Crohn’s & Colitis: A Comprehensive Naturopathic Guide for Complete Digestive Wellness (with a nationally-known naturopath, Jessica Black, ND). Our book has helped so many people afflicted with Inflammatory Bowel Diseases, part of the growing auto-immune diseases that cause diarrhea, bloating, nausea, vomiting, and cramping. These inflammatory bowel diseases, and other auto-inmmune disease are on the rise exponentially across the world, especially in the developed countries where processed food is available.
Think about it: There are certain behaviors that cause body/mind stress: We address this in the book, but I want to tell you that I am a patient/survivor of a stress-induced flare-up in 2006 that almost killed me. On my 5 foot 8 frame, I weighed 117 pounds. I spent a month at Dartmouth Hitchcock Medical Center. I was 45 and very sick, with 3 children at home and a business to run.
Stress was the way I worked, and I was on autopilot without taking time for myself. That has all changed, and I have been in clinical remission for the last 7 years! Let me tell you more….
As many readers know, I went to the Mayo Clinic in Rochester, Minnesota this past May to have a complete second opinion. I spent two days of my weeklong stay, at the wonderful stress reduction clinic.
~
Here are some of my tips gained from my research, and how I try to keep my disease in remission:
STRESS
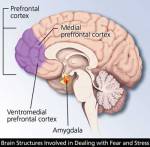
 A lot of us have low level stress. Most of us don’t live in the hyper-aware world, and we suffer the autopilot behaviors that contribute to what I call “the slow burn of stress response.” Our heart rate and blood pressure might be elevated, and our breathing and muscle tension is like this — shallow breathing and knots in muscles. There is an area at the base of the brain called the amygdala. This is the seat of our emotional reactions, or “flight of fight” response to stress. Many Americans live with this elevated, but low level elevation daily… a little bit of “Flight of Fight” stress is really okay, but not on autopilot.
A lot of us have low level stress. Most of us don’t live in the hyper-aware world, and we suffer the autopilot behaviors that contribute to what I call “the slow burn of stress response.” Our heart rate and blood pressure might be elevated, and our breathing and muscle tension is like this — shallow breathing and knots in muscles. There is an area at the base of the brain called the amygdala. This is the seat of our emotional reactions, or “flight of fight” response to stress. Many Americans live with this elevated, but low level elevation daily… a little bit of “Flight of Fight” stress is really okay, but not on autopilot.
Look at our brains — In our pre frontal cortex, there is an area responsible for relaxation, and it is not easy to stimulate and not an adrenal release, as per the amygdala part of the brain.
~
First we need to be aware of this pre frontal cortex We have to explore our own behaviors and habits, break out of autopilot, and participate in a personal practice. There are some things you can’t control, like weather or traffic jams; however there are some things we can control, and are important… An example from the workshop was if you have an overbearing mother (don’t worry, Mom, not YOU!), and how you need to take care of yourself first and use the excuse of health, and scale down. Awareness helps, and limit your exposure to stressful people and situations. It’s a process… keep boundaries in your mind, but “caring boundaries.”
Unhealthy responses to stress in our life are anger, etc. It is important to develop a healthy exercise routine, learn and use relaxation techniques (see below), and take care of yourself. This neural pathway gets easier and easier to tap into (see diagram at right). For example, my body knows and relaxes immediately when I walk into my home “yoga area” where I have a TV, and a carpet with a yoga mat. I use Rodney Yee’s DvD, “AM/PM Yoga,” and do the exercises every day… it gets easier and easier to tap into the relaxation part of my brain, and it is replenishing.
After a stressful day:
- Call a friend
- Laughter
- Read a book
- Knit
- Walk
- Walk the dog
- Ride a horse
- Volunteer at a soup kitchen
- Play the piano
- Do some gardening
In order to break out of autopilot, do a few things on this list on a regular basis.
~
Benefits: Concentration, Problem solving, Sleep…
We need to be participants: This involves “letting go of the wheel,” loosening your grip, and takes time and experimentation.
In the wonderful workshop, our instructor gave the analogy of flying on an airplane, and how you put the oxygen mask first, then help the child.
Talk therapy is another way to help relinquish the autopilot lifestyle… A regular monthly session with a trained, recommended therapist will do wonders for helping to care for yourself, establish boundaries, and feel safe.
Evaluate your stressors and prioritize your time, as you move forward in the break from autopilot.
Give yourself permission eg., “Be kind to yourself and ask for help.”
Often we don’t think about our career as a choice made for healthy reason, and it might be time to reevaluate what we do for work.
It is important to spend time with friends, develop hobbies…. Hanging out with people who make me laugh is a goal. A hospital study involved a control for two groups with the same malady: One group watched funny movies every day, and got out of the hospital faster.
It’s a process, and it is important to practice positive self talk.
—-
Start a simple practice of Tai chi and chi gong
Walk around with a gentle smile on your face and try to share it with strangers—you use less muscles and tension when you are not frowning, which can contribute to an overall sense of well-being and a way to focus on releasing the internal stress caused by being on autopilot…
I have found this “small smile” technique that is practiced by Amit Soud, MD, the head of the Eastern Medicine Section of the Mayo Clinic to be essential as a way to lessen internal stress.
~
TAI CHI AND CHI GONG: These ancient exercises are easy and relaxing, often available in small towns across the United States. For example:
We breathe with about 40% of our lungs. If we can learn to take slow diaphragmatic breaths, we can effortlessly lesson our stress levels. These exercises are the foundation and essential for relaxed breathing.
A simple exercise I learned at the Mayo Clinic:
Take in a slow deep breath,
and fill your lungs so even your belly sticks out;
hold for a couple of seconds;
pretend you have a lit candle and exhale
so that the candle flickers.
Note to reader: it might take 8 weeks or so to start seeing results.
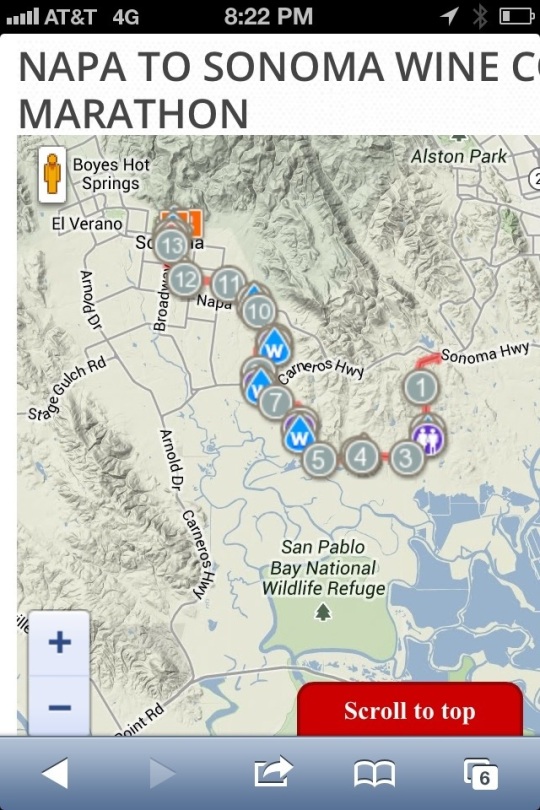
My second Team Challenge Half Marathon was a wonderful event! We arrived on Friday, and Saturday morning I met up with my old college roommate, and we went out to Point Reyes National Seashore.
The night before the race, we had a pasta party, and two inspirational speakers living bravely with IBD (inflammatory vowel disease) spoke— Saskia Madison and Michael Ginzberg. Since I am from Vermont, my state is too small to have a state team, so I am on Team Challenge from New England. We wore our special “Boston Strong” T-shirts. Team New England raised the most money of all the teams, over $400,000.
I also ran for Ryan McMahon, a former team challenge runner who was injured in the Boston bombing. I am part of a group called Run for Boston (#runforboston), and I am motivated to raise awareness for running as well as to raise awareness for the increase in inflammatory bowel disease worldwide.
There were teams from across the US to raise money for the Crohn’s & Colitis Foundation of America: 2.4 million was the total, of which 80% goes to research. I’m quite proud to be a part of this wonderful organization.
Race day, we got up at 4:30 a.m. to have breakfast and meet the bus to take us to Napa. We all congregated at a wine vineyard there — and there were over 3,500 runners—630 were from all the Team Challenge state chapters.
Before the start, people lined up along the vineyard road, and when the gun went off it took a long time to get moving — especially back where I was pacing myself at 11-12 minute miles!
We finally got moving, and took a left for the first leg of our route that went uphill pretty steadily for around a quarter mile. At the crest of the hill, I was amazed to see a long line of brightly-clad runners as far as the eye could see.
On either side of the road and the mass of runners, there were rows and rows of grape vines. In the distance, as the morning fog was rising, I could see the Mayacamas mountain range rising up from the floor of the Napa Valley.
There were mile markers, and water stops along with port-o-potties along the way. It was so pretty with the grapevines, and some beautiful old wineries, that didn’t really seem too arduous.
By mile 6, I ate one of my Cliff bars, and started to feel a little tired. But they had live music, mocha shots, and Gatorade, so it wasn’t too bad.
I just kept a really steady pace, and I listen to a lot of music, and that really helped my motivation.
Around mile 10, there was a stand on the side of the road, and two men were giving away glasses of Guinness beer.
At mile 11, one of my coaches, Dave, ran with me for a while and that was wonderful. The coaches for team challenge are amazing!
Soon after, there was a place where you could get glasses of wine, and that was pretty fun, but I didn’t get any— for fear of getting a headache!
At mile 12, we turned right and entered the small city of Sonoma. At this point people were lining the street, and urging us on, which was great. Both of my calves cramped up pretty badly, and I was kind of nervous. I could see the finish line ahead of me, and I thought I might have to sit down and not finish!
When I was within a few hundred yards from the finish, a coach from Seattle named Chris came along and ran with me — he could tell I was really pretty exhausted.
He was very calm when he told me to just take it easy and run slowly to the finish line, and then walk it off, which I did.
I have to admit, I did get a little choked up when I crossed the finish line, and I felt really proud of myself for living with Crohn’s disease yet still living my life to the fullest.
I’m still trying to make my fundraising goal—I have until August 21st and it’s a great cause!
I met so many amazing people through Team Challenge, many of whom are a lot sicker than I am. It is really inspiring AND fun. I really recommend this!
 A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
Crohn’s is not easily deterred. I was so lucky to have seven years of clinical remission. It was only in the last year, that my disease spread. My last seven years have been filled with hope and health, and it is easy to fall into despair when the doctors tell you that your disease has gone from nonexistent to “severe.”
~
Rather than saying “Woe is me,” and spending time feeling sad and useless (I did a lot of that, believe me), I decided to take action, and try to live the words of the Dalai Lama:
“Scientists say that a healthy mind is a major factor for a healthy body,” His Holiness said. “If you’re serious about your health, think and take most concern for your peace of mind. That’s very, very important.”
That said, I am on my way to health, for sure—no time to sit on my cushion meditating (I do that daily for a few minutes still); rather, I need to stay focused and take care of my body: better food, sleep, stress relief, education, awareness, team building, satisfying work, making money enough to live on, giving back to my community and the world…working for peace, justice, and environmental sustainability. According to His Holiness the XIV Dalai Lama, peace of mind is essential for health—words to live by.
This new diet, very much like The Paleo, is giving me strength and vitality. It is not for everyone—and I always tell people you must proceed with a doctor’s knowledge, for Crohn’s and UC can be serious, even fatal, if not managed correctly. I have worked really hard to form a collaborative team—my own book’s co-author, Jessica Black, ND, is my stalwart supporter and her book, The Anti-Inflammation Diet and Recipe Book has just come it in a second edition and has sold almost 100,000 copies! Jessie is an amazing health practitioner.
~
I have eliminated ALL grains and dairy from my diet—woohoo! What a difference. I found this great site, and I can use almond meal flour (also coconut flour), and I eat fruits and veggies, nuts and animal protein pretty much non-stop. I had an adjustment for the first week, as I really missed my oatmeal in the morning, but as you can see from the photo, my morning meal is wonderful and tasty, too.
I hope this post inspires people to look at their own diets, and proceed with caution (this diet is not recommended if you have flare-up symptoms of Crohn’s or ulcerative colitis). I began this diet with no symptoms, and after the first week, I started to feel like I had more energy, and my stress levels are kept low by walking 4 miles a day and sleeping 8 hours per night.
I’ll post some more photos of my wonderful meals… Summer is the best time to do this diet: only organic fruits and veggies and meat must be antibiotic-free, grass-fed…that whole thing! I buy all local meat, eggs, fruits and veggies… And I plan on putting up and preserving a lot of them this summer so I can continue summer’s bounty from my freezer (and canning room) during the cold Vermont winter!
I also have a nice little garden growing…. Kale, and more kale! Plus, tomatoes, green beans, lettuce, spinach, onions, asparagus, etc. growing your own food is another way to reduce stress and get physically fit—gardening is good for upper body strength!
Inflammatory Bowel Disease (Crohn’s & Ulcerative Colitis)
Our first-ever “guest post” on Dede’s blog! Drew and I “met” through Dede and Jessica Black, ND’s Facebook page, and Dede invited him to educate our readers and followers about the benefits of accupuncture. WTG, Drew! This is like a new book we should publish! A very thorough examination of signs and symptoms of Crohn’s and ulcerative colitis, along with specific treatment plans for acupuncture. Since Dede (seriously) is a wimp when it comes to needles (also, working on this using Ayurvedic treatment to help with this possible symptomatic “sensitivity” on the skin, which is very likely bowel, related, since the skin and the bowel ARE related!~)…Please welcome Drew, and share this, and come visit him if you live in the Southern California region—like our friends at the CrohnsJourneyFoundation.

This happy woman is like Dede, who hates needles, but has monthly acupuncture treatment—it really helps alleviate symptoms and detoxify the overworked liver, etc. when you have an auto-immune disease
Inflammatory Bowel Disease is a heading/umbrella that has other diseases underneath it. You may have heard of Crohns Disease, Ulcerative Colitis and Irritable Bowel Disease. You may know someone who’s been diagnosed with one of these or you may have had one of these unfortunate afflictions. In any case these can be serious debilitating conditions that sometimes require extreme care for severe cases but all require long term care. In this article I will discuss the differences and similarities between the three.
Crohn’s Disease: A chronic inflammatory condition of the intestinal tract was first described by Dr. Burrill B. Crohn in 1932, along with Dr. Leon Ginzburg and Dr. Gordon D. Oppenheimer. Mostly affects the end of the small intestine called the “Ileum” and the beginning of the colon/large intestine “Cecum” but can affect the entire length of the GI tract. Crohn’s disease can affect the entire thickness of the bowel wall leaving “skip lesions;” whereas, Ulcerative Colitis only affects the superficial layer of the large intestine.
Ulcerative Colitis: A chronic inflammatory disease that affects only the Large Intestine (aka: colon). The lining of the colon becomes inflamed, and ulcerations occur which bleed and produce pus.The inflammation and the ulceration lead to spasms, cramping/pain and frequent bowel movements.
Like Crohn’s Disease Ulcerative Colitis is an autoimmune disorder where your body attacks itself.
Crohn’s Disease
Symptoms related to inflammation of the GI tract:
• Persistent Diarrhea
• Rectal bleeding
• Urgent need to move bowels
• Abdominal cramps and pain
• Sensation of incomplete evacuation
• Constipation (can lead to bowel obstruction)
More severe symptoms:
• Fissures in the lining of the anus (tears)
• Fistulas (tunnel from one loop of intestine to another or connects the intestine to the: bladder, vagina or skin)
Ulcerative Colitis
Symptoms related to inflammation of the Colon:
• Bowel movements become looser and more urgent
• Persistent diarrhea accompanied by abdominal pain and blood in the stool
• Stool is generally bloody
• Crampy abdominal pain
General symptoms that may also be associated with IBD:
• Fever
• Loss of appetite
• Weight Loss
• Fatigue
• Night sweats
• Loss of normal menstrual cycle
Types of Crohn’s Disease:
• Ileocolitis: The most common form of Crohn’s, ileocolitis affects the end of the small intestine (the ileum) and the large intestine (the colon). Symptoms include diarrhea and cramping or pain in the right lower part or middle of the abdomen. This type is often accompanied by significant weight loss.
• Ileitis: This type affects only the ileum. Symptoms are the same as ileocolitis. In severe cases, complications may include fistulas or inflammatory abscess in right lower quadrant of abdomen.
• Gastroduodenal Crohn’s disease: This type affects the stomach and the beginning of the small intestine (the duodenum). Symptoms include loss of appetite, weight loss, nausea, and vomiting.
• Jejunoileitis: This type is characterized by patchy areas of inflammation in the upper half of the small intestine (the jejunum). Symptoms include mild to intense abdominal pain and cramps following meals, as well as diarrhea. In severe cases or after prolonged periods, fistulas may form.
• Crohn’s (granulomatous) colitis: This type affects the colon only. Symptoms include diarrhea, rectal bleeding, and disease around the anus (abscess, fistulas, ulcers). Skin lesions and joint pains are more common in this form of Crohn’s than in others.
Types of Ulcerative Colitis:
• Ulcerative Proctitis: For approximately 30% of all patients with ulcerative colitis, the illness begins as ulcerative proctitis. In this form of the disease, bowel inflammation is limited to the rectum. Because of its limited extent (usually less than the six inches of the rectum), ulcerative proctitis tends to be a milder form of ulcerative colitis. It is associated with fewer complications and offers a better outlook than more widespread disease.
• Proctosigmoiditis: Colitis affecting the rectum and the sigmoid colon, the lower segment of colon located right above the rectum. Symptoms include bloody diarrhea, cramps, and a constant feeling of the need to pass stool, known as tenesmus. Moderate pain on the lower left side of the abdomen may occur in active disease.
• Left-sided Colitis: Continuous inflammation that begins at the rectum and extends as far as a bend in the colon near the spleen called the splenic flexure. Symptoms include loss of appetite, weight loss, diarrhea, severe pain on the left side of the abdomen, and bleeding.
• Pan-ulcerative (total) Colitis: Affects the entire colon. Symptoms include diarrhea, severe abdominal pain, cramps, and extensive weight loss. Potentially serious complications include massive bleeding and acute dilation of the colon (toxic megacolon), which may lead to an opening in the bowel wall. Serious complications may require surgery.
Causes and who’s affected:
As many as 700,000 Americans may be affected by Crohn’s Disease and Ulcerative Colitis. It is equally common in men and women and while it can affect a person at any age there is a higher risk during the years from 18-35. The cause of IBD is not fully understood but there is a connection between diet and stress; as well as hereditary, genetics and/or environmental factors that play a role in the development of IBD. Studies have shown a greater risk of 5-20% increase in someone acquiring this disease if a “first-degree” relative (parent, child, sibling) has it and an even greater chance if both parents have an IBD. Crohn’s is most common among people with Eastern European backgrounds and it is increasing in number for African Americans. Ulcerative Colitis is more common among Europeans with a Jewish background heritage.
The environment that you put yourself in plays an important role as well. The occurrence is higher in “developed” countries than in “underdeveloped countries, higher in urban areas rather than rural, and in northern versus southern climates.
Treatment with Chinese Medicine:
 Due to the differential diagnosis that is applied in Chinese Medicine there are different “patterns” that exist when dealing with a disease. This is a similar idea to the different types of Crohn’s Disease and Ulcerative Colitis described above. However, with Chinese Medicine, the patterns are based off of the symptoms the patient is currently experiencing as well as their history, their facial color, body odor, general demeanor, abdominal diagnostic, pulse diagnostic and tongue diagnostic. All of this information is compiled which leads to one of many “diagnostic patterns” to which the according acupuncture points, herbal formula, diet and lifestyle is prescribed. Chinese Medicine is a powerful therapy that can help treat severe cases and help keep mild cases and patients who are in remission stay in remission.
Due to the differential diagnosis that is applied in Chinese Medicine there are different “patterns” that exist when dealing with a disease. This is a similar idea to the different types of Crohn’s Disease and Ulcerative Colitis described above. However, with Chinese Medicine, the patterns are based off of the symptoms the patient is currently experiencing as well as their history, their facial color, body odor, general demeanor, abdominal diagnostic, pulse diagnostic and tongue diagnostic. All of this information is compiled which leads to one of many “diagnostic patterns” to which the according acupuncture points, herbal formula, diet and lifestyle is prescribed. Chinese Medicine is a powerful therapy that can help treat severe cases and help keep mild cases and patients who are in remission stay in remission.
Before we discuss the differential diagnosis, there are a few terms that need to be explained. First one is the “Organ” system. In Chinese Medicine each organ is attributed to specific functions that don’t necessarily match a scientific viewpoint. For example the “Spleen” and “Stomach” are considered to be in charge of the digestive functions and water metabolism in Chinese Medicine. The “Spleen” actually handles some of the function of the “Western” spleen, pancreas and small intestine. The “Liver” has to do with the free flow of qi, which is easily obstructed by stress, emotions, diet and lifestyle. The “Kidney” can be attributed to water metabolism, as well as genetics and our “reserves.” The term “burning the candle at both ends” is a great way to describe how stress and lifestyle can damage the Kidneys. The “Heart” has to do with our emotions and deals with blood. When the digestive system isn’t absorbing food properly we cannot produce the nutrients and blood needed to support these organs. “Heat” refers to inflammation and “Dampness” refers to water metabolism malfunction. Both of these can manifest in numerous ways, as you will see below.
Below are examples of some different patterns that could be “diagnosed” as Crohn’s Disease or Ulcerative Colitis and what the treatment principle should be.
• Spleen Qi Deficiency: Intermittent dull abdominal pain that is alleviated with pressure, abdominal distention, early satiety, nausea, loose stools or diarrhea, loss of appetite, waxy pale or sallow complexion, fatigue, weakness, shortness of breath with exertion, spontaneous sweating, dizziness, and light headedness. Might have mild bleeding of dark, purplish blood, or less commonly, red blood preceding or following a bowel movement; or black, tarry, sticky, unformed stools; or occult blood in the stool discovered upon routine testing. There may be other signs of bleeding, such as heavy menstrual periods or easy bruising.
- Tongue: pale and swollen, with tooth marks (or pale and thin with significant blood deficiency).
- Pulse: Thready and weak or moderate.
- Treatment Principle: Strengthen Spleen, supplement and elevate qi. Nourish Blood and stop bleeding.
• Liver Qi invading the Spleen: Recurrent Diarrhea which may be urgent and preceded by cramping abdominal pain. The pain is relieved following defecation. The diarrhea may alternate with constipation. Symptoms become worse with stress and tension or eating. There is a possibility of mucus and blood in the stool. Other signs and symptoms include abdominal distention, poor appetite, nausea, heartburn, indigestion, borborygmus, flatulence and belching, which relieve abdominal discomfort, hypochondriac discomfort, ache and tightness generally worse on the right side, irritability, depression, moodiness, shoulder and neck tension, temporal or tension headaches, cold fingers and toes, premenstrual syndrome and breast tenderness.
- Tongue: normal or darkish body, or pale, or with slightly red edges: greasy coat especially over the root (depending on the degree of heat, deficiency and Dampness.
- Pulse: Wiry
- Treatment Principle: Harmonize the Liver and Spleen, regulate Liver qi, Support and strengthen Spleen, Alleviate spasm and pain, and stop diarrhea.
• Blood Stagnation: Chronic Diarrhea with a feeling of incomplete evacuation or tenesmus. The stools may be purple or black, sticky or tarry. The diarrhea may alternate with constipation.Fixed and localized, sharp or stabbing abdominal pain (usually in the lower left quadrant) which is worse with pressure. Dark complexion, dark rings around the eyes and purple nails. Spider naevi or vascular abnormalities over the abdomen, face and legs (particularly the inner knee and ankle).
- Tongue: purple or with brown or purple stasis spots; sublingual veins dark and distended
- Pulse: wiry, choppy or thready.
- Treatment Principle: Transform and eliminate stagnant Blood from the Intestines.
• Damp Heat dysenteric disorder: Frequent, foul smelling, explosive diarrhea with blood, mucus and pus: the mixture of mucus and blood will vary depending on the balance of Heat and Damp.Burning anus, tenesmus, colicky abdominal pain, abdominal distention, scanty concentrated urine, red complexion, red eyes, dry mouth, and thirst (maybe with little desire to drink). In the early stages there may be fever and chills, headache and a floating pulse.
- Tongue: greasy yellow coat; with more Heat a red tongue body and a dry coat; with more Dampness, a thick greasy tongue coat
- Pulse: slippery and rapid.
- Treatment Principle: Clear Damp Heat from the Intestines and Regulate Qi and Blood, stop pain.
• Spleen and Kidney Yang Deficiency: Chronic and relentless diarrhea which is thin, watery and mucoid, and may contain pus and blood. In severe cases there may be incontinence of stools and rectal prolapse. The diarrhea is worse from exposure to cold and cold foods. Mild tenesmus or a dragging sensation in the lower abdomen, not relieved by diarrhea. Mild persistent abdominal pain, which is better with warmth and pressure. Loss of appetite, listlessness, fatigue exhaustion, depression. A waxy pale or sallow complexion, cold extremities, cold intolerance, weakness and soreness of the lower back and legs.
- Tongue: Pale and swollen with a thin white coat.
- Pulse: deep, thready, weak and slow.
- Treatment Principle: Warm and Strengthen the Spleen and Kidney Yang. Disperse Cold, transform Dampness. Astringe diarrhea and elevate qi.
• Yin Deficiency with Residual Damp Heat : Chronic diarrhea with small quantities of sticky mucus and blood. Frequent urge to defecate but often in vain. Mild lower abdominal pain, tenesmus, loss of appetite, nausea, dry mouth and lips, thirst worse at night, afternoon or tidal fever that’s worse at night. Heat in the palms and soles, nightsweats, flushing , emaciation, weight loss.
- Tongue: red or scarlet and dry, with a greasy or peeled coat.
- Pulse: thready and rapid.
- Treatment Principle: Nourish and supplement yin and clear residual Damp Heat. Nourish and regulate Blood and stop dysentery.
• Heart and Kidney Yin Deficiency: Recurrent mouth ulcers, which appear in clusters and tend to aggregate on the tongue or tongue tip. The ulcers are painful and hot, with a narrow, slightly swollen, mildly red margin. They frequently recur and persist for up to several weeks before resolving. Often of many years duration, the ulcers tend to be provoked or aggravated when the patient is stressed, anxious or upset. Nervous, anxious individual, insomnia, vivid dreaming, panic attacks, palpitations, forgetfulness, dizziness, tinnitus, lumbar ache, sensation of heat in the palms and soles, dry mouth and throat, night sweats.
- Tongue: red with little or no coat, redder at the tip.
- Pulse: Thready and rapid.
- Treatment Principles: Nourish Heart and Kidney yin. Clear Heat, calm the (spiritual) Shen.
Forms of treatment include acupuncture, herbal formulas (which can be taken internal or external), Massage/tuina, dietary therapy, exercise and lifestyle consultation. When we utilize and multiple forms of therapy results are seen at a rapid rate.
*Disclaimer: The information offered in this paper is not intended to diagnose but rather to inform the public about IBD and give a brief look at how Chinese Medicine looks at and treats IBD.
References:
• http://www.ccfa.org /
• Will Maclean and Jane Lyttleton, (2003), Clinical Handbook of Internal Medicine “The
Treatment Of Disease with Traditional Chinese Medicine” Volume 2 Spleen and Stomach, University of Western Sydney
One of our readers wrote recently, saying her arthritis pain was really hard to deal with . . . Here is Dede’s answer, and hopefully some tips for others who also suffer from the related symptoms of arthritis.
Arthritis pain? Oh, I have it, too!
Arthritis is such a drag. but remember: We are all in this together . . .
Here’s what you can try:
-
Daily morning yoga with Rodney Yee DVD called “AM/PM Yoga”
Take Omega 3 fish oil capsules 2 “softgel” caps up to 2-3 daily with food (use best brand, highest quality—Dede uses Metagenics “OmegaGenics/EPA-DHA 720”)
Take a lavender bath with candles nightly before bed and use Epsom Salts in the water
Eat the healthiest diet: no sugar, caffeine (if you must, water down coffee and green tea okay), dairy or red meat
Make an appointment with a physical therapist (insurance usually covers this!)
Go to see an experienced acupuncturist (Chinese medicines best) and have 3-4 treatments in 2 months to see it it helps (make sure it is someone trustworthy with good recommendations)
Get a massage monthly to help cleanse and detoxify
Every time before your bath or shower use a dry Loofa sponge and brush your skin all over briskly to accentuate healthy cellular growth
Get 8-9 hours of sleep nightly
Use a castor oil pack to lay on sore joints—you can buy castor oil at a health food store, and Dede soaks a wool rag with it, to make a compress, then put SaranWrap over that, followed by a small towel, followed by a heating pad—ahhhh! The pain miraculously fades away, and you are forced to sit still and can read a book. Or, even better, you can meditate while you heal.
Walk 3-4 miles every day to clear your mind and keep your joints fluid and muscles strong to support the bones
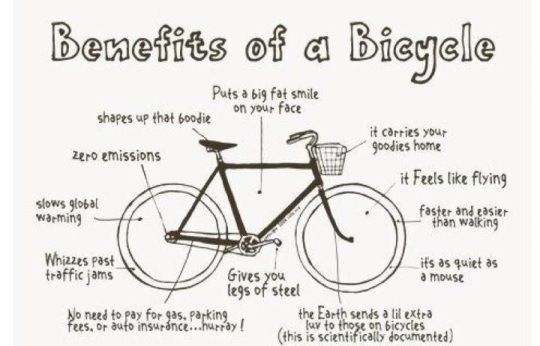
Ride a bike for cross training — great for quad strength, and it is easier on arthritic knees…
Monday is the “Living With Crohn’s & Colitis Bicycle Challenge”!!! Get out there and start pedaling—post photos of you on a bike on our Facebook wall, and “Thnk Pos!”
Most research on digestion, and the associated bowel diseases that are unfortunately on the rise in the world, starts with food and chewing. They talk about the act of chewing (mastication), and how the food is broken down with saliva, and goes down the esophagus, where it then enters the stomach and is further broken down (peptides and stomach acid)—then the slowly digesting food enters the small intestine.
We get the basic science of food and sustenance. I am interested in what happens INSIDE the small and large intestines, and why, for some of us, the microbial balance is disrupted resulting in bowel disease—which, in some cases like Crohn’s can be incurable and a lifelong struggle.
The small intestine is in fact smaller (in diameter) than the large intestine. It is where vital absorption of nutrients for the body’s health occurs. I think of it this way— to use a road biking analogy—if your tires are inflated, and the road is smooth, the inner tube is fresh and new, your feet are on the pedals and the movement spins the wheel with a steady and productive ease, then your digestive tract functions as it should. All antigens, are dealt with swiftly, and promptly, with the T-helper cells, and white blood cells, doing their job like a little army of white-suited patrols, following behind you like a bicycle sag-support wagon. The road is flat—no bumps, or traffic jams, or debris!
An antigen is any substance that causes your immune system to produce antibodies against it. An antigen may be a foreign substance from the environment such as chemicals, bacteria, viruses, or pollen. An antigen may also be formed within the body, as with bacterial toxins or tissue cells.
~
I won’t bore you with the details… But I did get into an argument the other day with my friend, Geoff. He tends to be a “know it all,” but then again, I pretend to be one, too! I said, “the digestive tract is longer than a football field!” To which he replied, “You’re wrong, and that’s crazy!” Together we looked on Google and found that the length of the digestive tract is about 20-30 feet, which is the WIDTH of a basketball court!!
Duly chastised, I began to ponder the sports field/court analogy, and the physical image/link to gut disease…. We, especially Americans, “get” the length of a court or a football field — soccer, maybe not so much! The physical representation, or image, of the digestive tract spread out in one long line across a basketball court makes me smile and cringe at the same time. I love basketball, don’t get me wrong! My daughter played D3 ball, and I am a big Carolina fan, but last night I was watching the Duke-Maryland game (Blue Devils lost!), and my mind occasionally saw a black line across the court. . . .
~
Now that we know the length of the digestive tract, let me add by saying the small intestine is much longer, and more vital to our nutritional health. There is an excellent research site and description of the process from a bio-chemical perspective here.
Below, is a description of the process of digestion, and note that in Celiac disease, the villi is damaged and does not function as it should. For those of us who most likely have what Dr. Kalish refers to as sub-clinical gluten intolerance, or Leaky Gut (damage to mucosal lining), it is imperative to strengthen our immune system which can become compromised: lifestyle changes, supplements, and Eastern medicine are all great ways to help us balance and strengthen our immune systems. For us Crohnnies, the actual wall of the small intestine is damaged, for uc-ers, the large intestine is inflamed and irritated, but can be removed to alleviate symptoms.
The small intestine is a long and narrow tube about 6 to 7 meters (20 to 23 feet) long. Food completes its chemical decomposition in which a compound is split into other compounds by reacting with water in the small intestine with the help of the liver, pancreas, and intestinal glands who pour their secretions into it. In the small intestine, there are an enormous number of tiny projections called villi, which absorb the end products of digestion. Villi and folds in the walls of the small intestine cover the lining and greatly increases the surface for absorption, which contributes to the length of the small intestine. The human small intestine has a surface area about ten times greater than the skin surface.
The large intestine is wider in diameter but shorter than the small intestine. It is only about 1.5 meters (5 feet) long. There is no decomposition of food in the large intestine. Bacteria in the large intestine break down any quantity of proteins that have not been completely digested. The large intestine is mostly used to store feces or waste, which consists of 10 to 50 percent of bacteria, undigested cellulose of plant cell walls, minerals, and water. This is then eliminated through the anus. (Physics Factbook)
The circular bicycle wheel image, for me, is much more compatible with my idea of the function of the small bowel. The large snakelike image of the width of the basketball court helps to justify the length in my mind, but the real process—that of digestion—is vital to our health, and it is our job to keep the tires smooth and running.
Happy spring everyone! Get out your bicycles, and tune them up! April 1st marks the beginning if the “Living With Crohn’s & Colitis Bicycle Challenge”…. Please post your progress here, and on our Facebook and Twitter pages—if you can’t ride, try walking every day!
Last, but not least, if you want to support me in my Half Marathon for the Crohn’s & Colitis Foundation (www.ccfa.org) this summer, please check out my fundraising page. I am excited to run with Team New England, and you can read why, here….
A new year’s tip from LWCC—start planning a small vegetable garden for spring! Just ’cause we (or someone we love) has Crohn’s or uc, doesn’t mean we can’t enjoy food and the delicate taste sensation of fresh herbs!
I am sitting here in my kitchen at home in Vermont, after a lovely two weeks of vacation spent with my family. As I was drinking my morning tea, I looked up and saw this:
So, what does this photograph mean? Right now, it symbolizes rebirth. I started the amaryllis before the holidays from a bulb…and now it is in peak bloom—hope; new life, new meaning…. But lest I wax too poetic here, I should note that a really determined chipmunk (probably the same invader of my garden last summer) is destroying my bird feeder as I write this! As I watch the greedy scavenger—the rodent—I think of the Hindu god, Shiva Nataraja, The Lord of the Dance:
The two most common forms of Shiva’s dance are the Lasya (the gentle form of dance), associated with the creation of the world, and the Tandava (the violent and dangerous dance), associated with the destruction of weary worldviews – weary perspectives and lifestyles. In essence, the Lasya and the Tandava are just two aspects of Shiva’s nature; for he destroys in order to create, tearing down to build again.
~
Since I found out I was in the midst of a severe flare up just six weeks ago, I have been plagued with fear that I will need surgery, have to take Prednisone again, and live again in the cycle of disease. Prednisone, especially, is a drug I hope I never have to take again—though I never got the symptoms of the round face, the bloating, etc,, I got the inner turmoil kind of symptoms: the frenetic feeling of gears winding up inside your body….not a good state to live in. Yes, those are the fears that lock us inside of ourselves when we are sick.
Well, not to dwell on that is easier said than done!
Here is a photo of my iPhone from when I was in Mexico last week…. As I lay in my hotel room bed for a whole day of fever and drifted in and out of consciousness, I put all the Spanish words for my disease in my “Favorites” in Spanish Dictionary, for fear I would have to explain to the hotel manager in case he had to call an ambulance to take me to the hospital (Merida was probably closest, but the hospital in Tulùm looked like a place for the bedraggled tourists to come to get treated for sunburns!). I was convincing myself that the flu I caught traveling was really a worsening of my flare up into a bowel obstruction.
My irrational fears were perhaps due to exhaustion and loneliness (my family went off to the beach ;(…. But I gradually realized that my fears were making me sicker! I always had trouble traveling when I lived with active Crohn’s-coltis for twelve years. We would pack our kids into the car, tents, camping gear, etc., and travel someplace like Okrakoke Island off the Carolina’s…..I remember that trip fifteen years ago, and being sick as a dog in bed for days, horribly bloated, and despairing the entire time…. I will never go back to that dark period of disease (though I hope to visit Okrakoke again someday in a normal state!), for it was a frame of mind that did nothing but foster the negativity around my life.
So, fast forward to hotel room in Tulùm. The cheerful towels our maid, Gabriella, created in animal sculptures, made me feel worse—their sweet little eyes stared out at me across the bed, and I felt they were mocking me — fever, perhaps?! After five hours of lying in bed and drinking nothing but water, and learning Spanish words about diseases of the bowel, I was ready for a change… I got up, showered, went out with my family for dinner, and my son helped me order a plate of the blandest food we could order at the restaurant, el Capitan.
Perfecto! I felt revived—chicken and vegetables will do that for me, along with a light cranberry juice (pure, no additives), mixed with mineral water. I thought the fact that I wasn’t moving my bowels was because there was a growing obstruction, when in fact it was due to the fact I hadn’t eaten much solid food in the last two days. It is amazing how illness, especially fever, will make us regress. We all want to be back in our mother’s bed with someone rubbing our forehead! My husband, who is not the most hovering-docile sort, was the practical one who said, “You haven’t eaten much at all!”
Well, that is my wisdom for the day…. Or is it wisdom? It seems more like common sense—keep the food journal going, and when you travel especially don’t forget it, or when you are faced with a new situation, like going off to college, or camp, or starting a new job…. It is essential for those of us who live with disease to be able to ask for help, but also to realize that our self pity might be making us sicker.
~
It is with that thought, and positive energy, that I want all of us to have in our Crohn’s & Colitis community as we move into the new year. “Think Positive,” was told to me by a doctor when I cried in my hospital bed, a few weeks before my bowel resection when I was overtaken by fear of the unknown and shaken by the heavy dose of steroids they had me on. A medical student, Dr. Osei Bonsu, DO, (currently an Internist in Galax, VA), was his name—and he held my hand and gave it a squeeze.
~
Now, back to planing my vegetable garden for spring planting….just a few months away.
Seems like my own health has taken a bit of a dive ;( … when I was freaking out about Lyme disease, it turns out it was a Crohn’s flare-up. Yes, I have been so happy to be in clinical remission for the past 6-1/2 years, I’d forgotten what it was like to have a flare up!
I thought I had Lyme disease, and was having stiffness and flu-like symptoms. Some of my readers will remember that I had a systemic flare of poison ivy during the first half of the summer (yeah, five weeks on Prednisone was not fun;( … Well, my dermatologist thinks the acute contact dermatitis (poison ivy resin is powerful stuff, not easily washed off and stays on your work gloves I learned!) caused my body to get out of balance, and I think she may be right! There is a strong connection between the skin and the gut — more on that subject in a later blog post.
I was at Dartmouth Hitchcock this week for a colonoscopy, and my results were very discouraging. My small intestine is in an active flare, characterized as severe. The news could have been better that is for sure! I am still in shock. My small intestine is riddled with Crohn’s in a 20 centimeter area just near the former surgery. Crohn’s is incurable and when it does this, they get serious and make you take these auto-immune suppression drugs. The recommended drug, 6-MP, is an immunomodulator – the way it works is it suppresses your immune system so that your own immune cells will stop attacking the lining of your intestines. There are patients who tolerate the drugs and it helps them stay in remission and pain free. Others have reactions to the drug, like fevers and stiffness. What the doctors look for at the beginning is liver damage.
On Thursday, after my colonoscopy, they got me right to the lab to draw blood for the test to determine if I could tolerate the 6MP. I, of course, started talking to my wonderful GI, Steve Bensen, about not taking the drugs. Couldn’t I work with my naturopath, I reasoned, and take the less toxic drugs she prescribes, and come back in 3 months for a scope? I did just finish a heavy round of Doxy for the symptoms of Lyme disease (for the record, I had an engorged deer tick that I pulled off and squashed and flushed down the toilet — always save the tick to be tested!), so the antibiotic had upset my stomach.
The head of the IBD Clinic, Cory Seagel, even came into my little curtained room with me in my Johnny gown sitting on the side of the bed. “You should start the drug immediately if your liver can tolerate it, better yet, you should take a combination of 6MP and Remicade,” he said.
Here is a good definition from Livestrong:
6-Mercaptopurine, or 6-MP, is a purine analogue antimetabolite drug that is used in the treatment of acute lymphoblastic leukemia, Crohn’s disease and ulcerative colitis. Purine analogues impair DNA synthesis, leading to less cells being created. Acute lymphoblastic leukemia, Crohn’s disease and ulcerative colitis are all conditions of an overactive immune system. 6-MP helps to decrease the amount of immune cells in the body to help control the disease.
The findings
The colon appeared normal. My sigmoid resection at 15 cm and its short blind colonic pouch had normal anastomosis (a term for surgical connection)….This is good news! Large intestine: check.
Ileal resection: segmental inflammation characterized by erosions, erythema, fir ability, granularity, loss of vascularity, confluent deep ulcerations, and serpentine and shallow ulcerations found in neo-terminal ileum and extended from my first surgery for 20 cm (about 8 inches)…. Small intestine: NSG (not so good!)
The power of poetry/intention
There is something about the language of medicine that I find vaguely hypnotic and poetic. Weird as it sounds, understanding the human side of medicine is an intention of mine, and one that I hope to impart on my readers, should they desire to learn more!
The path ahead
I wish I didn’t have this new problem, and feel fine! I went 5-10 years last time, but this time the wall of the small intestine is compromised and thinning. I may be flying out to the Mayo Clinic, for a second opinion and work-up involving their more integrative approach. I am a wreck about this, of course, but trying to stay focused. As my daughter, Emma said, I have such resolve and a positive attitude… Don’t feel like dwelling on it too much, but wanted to let my (our) wonderful readers know why I’ve been out of touch. I am going to start with the naturopathic doctor on Tuesday….. and Mayo Clinic, probably in January.
Notes from Jessie Black, ND
Let’s work with an accompanying pharmacist and try low dose naltrexone — start very low and amp up to 4.5 milligrams. In addition, she mentioned a very powerful high-potency coated turmeric (this is hard to absorb, so it’s necessary to work with a naturopath who knows their herbal medicine), and a new, more fiscous fiber called PGX. Fiber is something I take daily, already, along with garlic, Aloe Vera, extra C, D vitamins, calcium and multi-vitamins and Omega 3 capsules. A good article about helpful herbs is found here

Dede in the recording studio at VPR. I am happy when I am writing!
My basic diet now: No caffeine, dairy, processed foods, alcohol and trans fat. Instead SCD-certified food, lots of fresh-steamed veggies, cold water fish, and other foods from SCD! An awesome site for basic dietary help is found here! Link to a flare-up diet.
This blog will detail my journey. Thanks for your support and being part of it all! I welcome comments and suggestions, especially from IBD sufferers who have taken other meds besides 6MP and Remicade. Or IBD patients who have taken the drugs and had good results…I want to examine and research both options, along with a more integrative approach to possibly even healing the current severe inflammation without drugs!
I will start off by following my co-author and naturopath, Jessica Black’s Anti-Inflammation Plan (diet and lifestyle) that is in our very own book, Living With Crohns & Colitis!
- caffeinated beverages
- fried foods
- processed foods
- peanut butter
- carbonated soda
- citrus
- wheat
- pork
- tomatoes
- potatoes
- dairy
- sugar
- eggs
- shellfish
- peanuts
- anything that contains hydrogenated oil
After four weeks, reintroduce the eliminated items, one per week and if no allergic symptoms occur, add the item back into the diet. Read more More to come….
Blessings, Dede
Since my garden is starting to produce, I have felt more empowered to eat healthy. It is kind of a no-brainier that growing your own food is rewarding, cheaper than buying, and it also gives you a good workout (like try turning over a garden bed and weeding, for some arm-toning work!). I found this video recently in my research, that is excellent, and I am very interested in the Japanese study cited by Dr. Michael Gerger (I checked out his other videos, too, on http://wwwnuitritionalfacts.org.) about becoming a vegetarian, and the benefits for those of us with IBD. Exciting results….and being a partial vegetarian isn’t that bad . . . Read on!
~
Decrease Inflammation through Diet and Lifestyle Canges
Likewise, dietary goals to help us cope with Inflammatory Bowel Disease are always on my mind since I wrote the book with Dr. Black. I want to share with you some of the recent changes in my diet, and how it is helping quiet my gut and make me feel better and more energized.
No Red Meat
First thing: don’t eat hamburgers! I LOVE them, and can add them to the list of foods I gave up, and miss a lot (in case you are wondering: pizza, bagels, and a grilled burger with melted cheddar cheese…..).
Rather than feeling sorry for myself, while my husband grills his burger, I switched to Amy’s (TM) brown Rice crust pizza, rice cakes instead of bagels, and Gardenburgers (TM) instead of hamburgers (on the grill with some low-fat cheese and topped with a slice of Spelt bread).
Lighten Your Dairy Load
Switch to yogurt! In Breaking the Vicious Cycle, Elaine Gottshalk recommends making your own yogurt, but if you can’t, you can buy a high quality brand, like Stonyfield Farm 0Fat yogurt, and switch to lowest fat cheese, like Feta, pecorino Romano, part-skim and aged cheese, for just a few examples. There are some great lactose-free products on the market. Here’s a good article from Everyday Health to support this.
Now What Do You Eat?
Call me crazy, but I love this question! No wheat, no red meat, (note that I am able to digest dairy pretty well), and limited dairy….INCREASE fruits and vegetables. This is the plan! And the garden—wow!—my little 3 x 10 foot raised beds are producing like crazy now. (See attached photos of my two humble raised beds, packed with yummy veggies and flowers you can eat and also to keep pests away.)
Even our First Lady, Michelle Obama, is into the family’s vegetable garden—there is even a new book out about it, with recipes (I found a very funny review in The Daily Beast!).
And, it isn’t that hard to do—all you need is to add some good organic composted soil mix, and some starter plants like tomatoes, basil, lettuce, kale, broccoli, scallions, and Brussels sprouts, maybe some snap peas and cucumbers, and, voila! You have a garden!
What can we do going forward?
Grown your own food, and commute to work via metro, bus, or carpool; or better yet, ride your bicycle or walk. Rather than sitting around complaining about how hot it is, try riding your bike or walking in the early morning, before the heat gets oppressive, have your shades drawn during the day to keep your house from overheating, etc. Start small, and you will feel like you ARE making a difference. This summer, it is hot, dry, humid, and there are countless areas in the world showing record-setting droughts, heat waves, etc. With environmental activist, Bill McKibben sounding the alarm, (see this excellent article in the Guardian), people are starting to listen. The whole Eastern seaboard of the United States is at risk from tropical storms and rising sea levels, in just “one” example of how burning fossil fuel is contributing to the heating up of our planet.
We must adapt environmentally, as well as health-wise: inflammation being the byproduct of idiopathic (no known cause, no known cure) diseases like Crohn’s, colitis, IBS, etc.