Recently, on Goodreads, a reader wrote a very thorough review . . . It makes me think I should just do a book of all of “Dede’s Grey Boxes” from the Crohn’s book! What do you all think? A “how-to” from a patient who has kicked Crohn’s disease? A “saying no” to major medical institutions (like the Mayo Clinic) who advised me to start medication (Remicade/Humira, etc.) immediately and I didn’t and I beat the disease by following a naturopathic/holistic health plan that was outlined in our book . . . (just to be clear: Allopathic medicine saved my life by a combination of prednisone and bowel surgery of my small and large intestine (about 2 feet) to keep me alive…)
Check out the review & Happy Spring! Maybe I will work on this new book if it will help people!
~Dede
Living with Crohn’s & Colitis: A Comprehensive Naturopathic Guide for Complete Digestive Wellness
by Rebecca
Recommended for: People with Crohn’s, Colitis, IBD and their loved ones
Having just had a bad flare up of my Crohn’s, and a long and scary stay at the hospital, I’m now on a mission to read up more on current healing and overall wellness for people in my situation. This book was the only one amongst a sea of books that I had any interest in reading as a jumping off point. The combination of medical and personal account in this book is incredibly helpful. Hearing accounts of those who have “been there, done that, got better!” really is a spirit lifter for someone coming out of a bad flare and wanting to get on the right path.
The clinical information in this book is spot on and seems highly up to date. The biggest part of which is the proliferation of the idea that diet does matter to this disease. I was utterly dumbfounded during my hospital stay when I was given a menu of items I was allowed to eat (after being off food nearly a week) and it included so much junk. Though I didn’t thoroughly question my multiple doctors on their stance of diet in relation to Crohn’s, I got the impression most of them are operating under the “it doesn’t really matter what you eat” mentality. This blind spot in medicine, and not just related to Crohn’s, is a huge failing of our current system, and getting doctors to work with you on natural healing can be a challenge. Thankfully, books like this one are out there to help people start to see the interconnectedness of things like food, stress, supplements, along with pharmaceutical drugs and “modern” medicine. I have to give this book 5 stars for being detailed but understandable, informative, up to date accurate, and personally relate-able. The tips and tricks through the book are easy to understand and begin to incorporate in a healing plan for yourself. I recommend keeping paper and pen nearby to write down the names of various healing methods to try (like acupuncture and massage), as a reminder to look up that sort of thing in your area, and write down the names of supplements, foods and meals to try, etc.
My only complaint about this book is that Dede’s story and a lot of the helpful information is incredibly scattered throughout the book. We get chunks of things here and there between the related medical information. It was fine when reading through the first time, but I think the book would benefit from a few sections at the end that sort of combine the snippets scattered throughout into a more cohesive “summary” type section at the end for easier access when you want to use this as a reference instead. This is truly minor though, and since I can easily search the book on my Kindle it isn’t a huge deal to go back to re-read.
This book is a most excellent jumping off point for anyone wanting to get more information about Crohn’s and Colitis and a path to begin healing the whole body, not just covering up symptoms.
~~~

Based on my experience with having an autoimmune disease, I have created the following list. Think of it as a kind of spring cleaning. Remember everyone is different, so some of my tips may not work as well for you but it’s worth a try (and as most of my readers know, I recommend keeping a daily log of your diet and activities and stress level). Here are “Dede’s daily tips” as follows:
- You should eliminate all sugar from your diet.
- They say no alcohol or coffee, but maybe a tiny bit of black tea, or half a cup of coffee with boiling water a day. I also have one or two drinks over the weekend. Vodka tonic or gin and tonic; sometimes I have a light beer.
- No dairy. That said, I do allow myself 1 tablespoon of half-and-half in my tea or coffee per day. That’s my only luxury!
- No grains at all! Focus on big salads (with avocado and organic vegetables and a hard boiled egg in the mix—make your own dressing with pure olive oil and a little bit of lemon juice or balsamic vinegar)), and chicken, fish and eggs (all organic and the fish should be cold water/wild caught), and chopped nuts and dried fruit.
- Start drinking green, organic Moroccan mint tea in the afternoon for a little pick me up, and snack on carrots and hummus. At night, always drink a cup of chamomile tea with a little honey. This will help you de-stress your body. And mind.
- Try to get out and exercise, usually walking (or slow jog), 3 miles per day. When you come back, do gentle Rodney Yee yoga for about 20 minutes, and then do guided meditation for about 1 to 5 minutes. When you do guided meditation try to focus on healing and forgiveness and bring the breath from the top of the head down the spina. Focus on the breath. I always do a cleansing mantra that goes like this: white light healing inflammation gone.
- Try to get at least seven hours of sleep a night
- Take a hot bath or shower and use lavender in the bath before you go to bed. Try to read a book before you go to bed to take your mind off social media, etc.
- Get acupuncture once a month. Get a massage once a month (I know this is expensive, but it’s worth it!)
- Take a really good quality probiotic every night before bed. I usually take the Jarrow brand with the highest count of lactobacillus and acidophilus.
- Take omega-3, a multivitamin, vitamin C, hi high-potency turmeric/curcumin, and some liquid vitamin D drops every day.
- When you feel a tiny bit of a scratchy throat or rundown, add an immune booster homeopathic liquid (usually it’s about 30 drops in water) once a day before going to bed. Note: when I’m really feeling sick, with actual symptoms like cough or fever, I take goldenseal and echinacea in liquid drops.
- Carry a small spray canister of Bach Flower Remedy in your knapsack or purse. When you really feel rundown or stressed, just spray twice in your mouth. It really helps!
- As far as this list goes just try it for three months and see if it helps, then continue for three years (!). But really do it carefully! You can make things using almond flour and coconut flour (homemade tortillas, yum—black beans are okay in moderation and I mix them with roasted veggies/roasted potatoes).
- I forgot to mention that I love coconut milk—unsweetened—that you can use for breakfast. I usually mix bananas and nuts with dried fruit and cut up melon or strawberries in a bowl and add coconut milk to make a kind of morning cereal.
- Drink tons of water every day as well! I think that’s it… but I hope it helps.
Try to plan some kind of trip, and remember, it doesn’t have to be expensive or involve air travel which can add to the stress. Just a trip to the beach or a hike with a friend or loved one is a great way to relax. Going out in the woods every day is amazing.
👣🌱👣🌱👣
Happy Spring! I would love it if readers shared their own tips in the comment area.
Blessings,
Dede
According to the Mayo Clinic, after you eat, it takes about six to eight hours for food to pass through your stomach and small intestine. It takes a total average time of 43 hours from eating to stool elimination—I like that they call,this “transit time.” Food then enters your large intestine (colon) for further digestion, absorption of water and, finally, elimination of undigested food. After I researched this topic, I thought about how proper digestion is integral to maintaining good health — vital, really. I am interested in hearing from readers about exploring their own relationship to food. Start when you were young, or when you were first diagnosed. I recently discovered the amazing work of Crohn’s patient, Daniel Leighton. He openly explores his disease through his art, and I was blown away—his piece entitled “Tied Up at the Hospital” is superb (heartbreaking to me), and I encourage you to follow his work. So, let’s use ART to share our experiences! I use creative nonfiction, and writing has always been my release—in our book, Jessica and I encourage patients to “keep a food journal,” but now I also want to encourage patients to explore their disease, their relationship to food, their fears and loneliness, humor and love, through making art (photography, poetry, writing prose, painting, video, drawing, etc.). I can’t wait to publish some of these works! (Email me at dede.cummings1@gmail.com.). Okay, I will start off with a piece of my own creative nonfiction:
How my longing for food — my lifelong love affair with what I could, or could not, eat — began.

I was longing for food, literally desperate for the half-eaten slices of pizza left on the plates at a restaurant off Harvard Square. I was a 26-year-old bulimic, and food was my secret obsession. Who doesn’t love the hot-out-of-the-oven, doughy-crust pizza with fresh-grated mozzarella garnished with chopped basil leaves?
The revelers had straggled out of the room after a private engagement party. I told my boyfriend I had forgotten something, and walked back in through an arched doorway. The jukebox finally playing the Bonnie Raitt song, “Somethin’ to Talk About,” I had selected earlier. I stood there and gazed around the room: it looked a hurricane had breezed through around 60 knots with chairs overturned and crumpled napkins scattered about….
But it was what was on the paper plates that caught my attention: I made my way along the tables and grabbed slices of pizza and—gazing back at the arched doorway to see if anyone was coming — I scarfed them down and pushed the food into my mouth with both my hands like a refuge from war-torn Biafra.
You see, I didn’t know it then, or perhaps that was when I knew something was the matter with me. I was skinny and sick; mentally obsessed with a longing for food that occupied my thoughts much of the time.
A morning run along the Charles River was the usual start to my day—I loved this and felt so light as I jogged the worn paths past the brick buildings of academia. After my run, my reward was half a honeydew melon and a cup of coffee. Then I’d ride my bike to work at the publishing house on Beacon Hill. At lunch, I ate dry salad, and when I came home in the early evening, I ate popcorn with brewer’s yeast with Diet Coke.
Why, you may ask, did this young woman who was outwardly happy—a job in publishing, a boyfriend who had returned after a year hiatus, a loving family in nearby Providence, Rhode Island—resort to eating leftover food from people’s plates in public restaurants?
Why, indeed.
Having a mother who apparently subsisted on candy bars was one thing, a father who talked obsessively about food and his inability to loose weight, was another. “Am I fat?” plagued me throughout my adolescence.
My family prided themselves on being thin and fit, with tennis, riding, and golf practiced at various clubs—and at school, we played field hockey. Going to an all-girls high school had the added benefit of questions like “You Haven’t Gotten Your Period Yet?”
After high school, I took a year off from attending the non-existent college that my parents pretended I’d been accepted to. I headed to Vienna, where Weiner Schnitzel, Würst, pastries, and beer were to form the main ingredients of my diet, and after a few short months, I weighed 170 pounds.
When I returned from Europe after a year, my father announced that I had gained the “Freshman 15-times-two,” without attending college!
#
I remember the day I landed at Boston’s Logan Airport. My mother and one of my little sisters, Alex, stood there at the gate. My mother had her kerchief on, covering her wig at the top of her head that gave her that ’70s bouffant look; she was wearing her big Jackie O shades and had one of those purses that look like a small picnic basket with flowers painted around the edges clutched under her arm.
“Guüten Tag, Muttie und meine kleine Schwester!” I called gaily.
I walked toward my mother and sister and watched their mouths drop open. I was around 180 pounds at that point, my hair was cut in an ill-fitting pageboy, and my skin was dark brown from a summer spent sleeping on the edges of fiords after hiking around Scandinavia. They had no idea who I was!
The reality of my situation—home after 12 months after living on my own in Vienna and traveling around Europe—was horrifying to me! I was so heavy the buttons on my Indian print button-down shirt were almost popping off.
The whole way home in the car, I only spoke German, trying to explain to my mother that I had “forgotten how to speak English!”
I also liked this “no food/empty stomach” feeling I had in the car that afternoon when I returned, a stranger to my family, back from my year off, and I wanted it to last.
I retreated to my bedroom and unpacked my Kelty backpack, holding back the tears that I knew would never come.
#
This piece is excerpted from Spin Cycle by Dede Cummings, a creative nonfiction work-in-progress to be published (hopefully!) in 2017.
What About Bowel Surgery?
There are various complicated surgical options available these days which continue to change and develop with the advancement of medical techniques and technology. If you are experiencing significant symptoms, or problems that either warrant immediate attention or have not responded to previous treatments, please consult your physician or gastroenterologist about surgical options that may be right for you.
Dede’s Story
May 22, 2006, I was hospitalized for three weeks for a dangerous bowel obstruction due to a flareup of Crohn’s disease. My surgeon, the amazing Horace Fuller Henriques, III, removed a large section of my Sigmoid colon along with an attached granuloma, and he removed the terminal ileum and cecum. After a really rough 24 hours with the pain aided by a morphine pump, I began to come back to the world. Horace came to visit me in my hospital room, and while I was in my groggy state, he excitedly told me how he had rebuilt the ileocecal flap. I felt like I was listening to an episode of This Old House on PBS—it was like he was discussing the carpentry job!
It is hard believe that was nine years ago! My quality of life improved after my surgery, so much so that I have remained drug-free and very healthy since then. Sure, I’ve had times of flareups, but I’ve never had to go back to the hospital or stay in bed for more than 12 hours. Since I’m so attuned to my body and keep a food journal, I can notice when flares are coming and I conveniently resort to my dietary and lifestyle regimen in order to stop the flareup before it really knocks me down. I take lots of daily supplements prescribed by my naturopath, too, like VSL#3 Probiotics and Zturmeric, along with Omega 3, Vitamin C, D, and other supplements.
Yesterday, a young mother of two who is a professional singer-songwriter, called me to talk about her case of Crohn’s and her upcoming surgery. I love it when people find me, reach out and email me, and sometimes call me. I feel that the Crohn’s and colitis community is a really tightknit one, and we have the CCFA to help through their efforts as well. But it is the people with Crohn’s, and colitis, the patients themselves, I want to hear from! We have had to endure so much and, in the case of Crohn’s, have had to live with a disease that has no cure. The very active reaching out – whether it’s by email or phone for text message – is a big first step toward healing and taking charge of living with chronic disease.
So back to surgery. . .
Surgery should be a last-resort treatment; but if the need arises, surgery may provide relief for some individuals. About 20% of ulcerative colitis suffers will require surgery at some time in the course of their illness. Approximately 75% of Crohn’s disease patients who have disease in the small bowel will have surgery in the first 10 years after diagnosis. Unfortunately, if no other treatment is done, nearly 50% (or more) of those who have surgery for Crohn’s will still have a reoccurrence of disease symptoms. In colitis that does not respond to medical treatment, surgery is an option that can wipe out the disease. Many people live without the large intestine. In my case, the risk of perforation of the small intestine was very dangerous. If surgery for Crohn’s disease is an option, it is much safer to have elective surgery, rather than be admitted like I was through the ER.
If you have a scheduled surgery for either Crohn’s disease or ulcerative colitis, I highly recommended having a lengthy pre-op appointment with your surgeon so you understand fully the outcomes and what to do and how to prepare. Since I rely heavily on the care of my naturopathic physician, I also scheduled a pre-op appointment with her, where she planned a whole course of preparation for me. This included taking Arnica before my surgery and doing meditations and preparations with diet to lessen the burden on my digestive tract.
After my surgery, the surgical nurses were instructed by my naturopath to place small pellets of Arnica underneath my tongue. It is still amazing to me that this big teaching hospital where I was a patient was so accommodating! Also, the hospital had a wonderful dietitian who helped me slowly introduce foods back into my diet — and made me drink Smooth Move tea! I remember my stepsister went to the local natural foods co-op and smuggled in some organic chicken broth. The wonderful Dr. Henriquez even searched high and low for someone to come in and do acupuncture for me, and there was also a volunteer at the hospital who was able to do Reiki (a form of alternative medicine through “hands-on healing” developed in 1922 in Japan) to aid in my recovery.
After five days, I was ready to go home. It wasn’t easy, and transferring from morphine to other pain meds was really difficult. I also got really depressed and cried a lot as I tapered off Prednisone (tapering should be done with great care, and slowly, so as not to cause a flare-up). But, I let my body gradually heal and realized that crying and being depressed is part of having major surgery, too. But I didn’t just pick up my life the way it was: my recovery lasted about six weeks and I took it day by day, and very slowly, and I asked friends to help with care for my kids and help with house cleaning. I kept a food journal and gradually added exercise every day, along with yoga and meditation.
So, don’t despair if you have a surgery coming up. Instead, take control of the situation and keep a positive attitude!
When you or your loved one was first diagnosed with IBD, you probably felt like your life and taking a sudden spiral downward. You may have found yourself in the state of utter confusion, a deep-seated feeling of loneliness and depression taking root in the very core of your being. This may sound dramatic, but too many sufferers of both Crohn’s disease and ulcerative colitis feel this way in response to their diagnosis. The good news is that the better informed you become about your newly diagnosed condition, the better off you will be in the long run.
One problem that many people with IBD know all too well, is that these diseases, especially Crohn’s disease, can reoccur. Although therapies can reduce signs and symptoms, often the hope for full remission is stymied by widely varying factors.
Treatment options often include hospitalizations, surgery, and medications, but they rarely include a holistic approach that incorporates acupuncture, a new diet (potentially wheat-and-dairy-free), stress reduction, psychotherapy, yoga and meditation, naturopathic medicine, and a special protocol in detoxification.
When the proper groundwork is set for healing, the treatments, lifestyle practices, and even pharmaceutical medications, are much more effective at reducing symptoms and promoting healing. Our bodies were meant to function as a whole, and treatment plans should always be directed at the whole body to achieve the desired effect of wellness.
For me, as a Crohn’s disease patient, I benefit so much from going to see my regular doctor (an M.D.), and my naturopath (and ND), as well as my IBD specialist at the clinic at Dartmouth. I hope that someday soon, all three will be able to work together seamlessly. Until that time, I have to be the instigator, and make sure that my medical records are sent to all three places, and I have to be very proactive to stay on top of my appointments, asking my questions, doing my own research, and creating my own support system. All of the specialists and doctors are very busy people (as most of us are), and it is imperative for those of us with IBD, or our caregivers, to be very motivated.
Sometimes it can feel overwhelming. But make a list of things to do:
- Walk every day—start small, and gradually add miles. . . . A walk on the beach, like my friend in the photo, really releases stress. Do a short yoga stretch before or after!
- Buy a new water bottle—I love my 22-ounce LifeFactory glass water bottle with the rubber exterior!), and take one step at a time.
- Find a recommended naturopath in your area.
- Make sure you have at least yearly appointments with all the doctors on your “team.”
- Embark on the new dietary guidelines in this book.
- Take a high-potency probiotic (I take 1 capsule daily, called VSL#3, that really seems to be helping by bowel movements), or one that is recommended by your team.
- Consider asking your MD or ND to do a complete blood work-up, and also to test your adrenal function.
- (Last, but not least,) Work with a naturopath, preferably, to balance the immune system to achieve homeostasis that is promoting wellness in your mind and body.
Happy Spring Detox and Motivation….. And Happy Almost Summer!

Most processed foods are not ideal for our health. These foods are often laden with artificial chemicals which can cause all sorts of havoc to our body. Whether you have Crohn’s or colitis, or IBS, now is the time to eat the healthiest diet possible—only fresh, local and organic. It is worth the extra money! Lots of vegetables, fruit, organic chicken and sustainably caught wild fish are good, too. Red meat that is grass-fed, organically raised is okay once in a while; local free-running chicken eggs, leafy greens like kale, nuts and dried fruit, too. No dairy. Coconut milk is good. (Source: Hungry for Change)
A recent study from Georgia State University published in Nature, points to emulsifiers leading to changes in the intestinal track that eventually lead to inflammation. Food addivitives are being suspected, and research will move forward from mice to human studies.
The intestinal tract is inhabited by a large and diverse community of microbes collectively referred to as the gut microbiota. While the gut microbiota provides important benefits to its host, especially in metabolism and immune development, disturbance of the microbiota–host relationship is associated with numerous chronic inflammatory diseases, including inflammatory bowel disease and the group of obesity-associated diseases collectively referred to as metabolic syndrome. A primary means by which the intestine is protected from its microbiota is via multi-layered mucus structures that cover the intestinal surface, thereby allowing the vast majority of gut bacteria to be kept at a safe distance from epithelial cells that line the intestine1. Thus, agents that disrupt mucus–bacterial interactions might have the potential to promote diseases associated with gut inflammation. Consequently, it has been hypothesized that emulsifiers, detergent-like molecules that are a ubiquitous component of processed foods and that can increase bacterial translocation across epithelia in vitro2, might be promoting the increase in inflammatory bowel disease observed since the mid-twentieth century3.
This study is good news for those of use who have a diagnosis of Crohn’s or colitis, collectively know as IBD.
~
I was diagnosed with Crohn’s disease in 2001, officially, and managed the disease with antibiotics, Prednisone, naturopathic doctor visits and supplements. No one else in my family suffers from Crohn’s. However, in 2006, I developed fistulas and a granuloma, and I was extremely sick when admitted to the hospital with a blockage in my small intestine (there terminal ileum is the most common place Crohn’s develops). I didn’t eat solid food for one month leading up to, and after, my surgery— I weighed only 119 lbs on my 5 foot 8 frame (now I am up to 145 lbs.!)
After returning home, I began to search for a book that would aid in my recovery and help me establish a “new lease on life.” Surprisingly, I couldn’t find this book anywhere—so I began to write a proposal to write the book that I was looking for: a book that would be predominantly a wellness guide about living with an incurable disease. Here is what my teacher/editor had to say about this book:
“Dede is an amazing woman! In this book you will find not only helpful advice but real inspiration.”
—Julie Silver, M.D., assistant professor, Harvard Medical School, author of What Helped Get MeThrough: Cancer Survivors Share Wisdom and Hope
At that time, I had had a moderate case of Crohn’s for eight years and had been in and out of the ER four times for treatment of flare-ups (usually fluids and bowel rest did the trick). I was ready to learn how to manage my condition and take a proactive role in my own health so that I could avoid more hospital stays and enjoy life and doing the things I loved again, like hiking, cross-country skiing, running, and especially traveling.
Now that the book is out, and my new cookbook just came out, I can say with confidence that Jessica Black, ND (my co-author) and I were certainly on the right track in terms of our research into gut microbiota! Jessica was already a forerunner with her wonderful book, The Anti-Inflammation Diet and Recipe Book. I really have Jessie to thank, for not only being my coauthor, my far-flung naturopath (I am on the east coast and she is in Portland, Oregon), but my inspiration for taking charge of my own health.
In our book, Living With Crohn’s & Colitis, Dr. Black and I frequently stress the need for an additive/preservative-free diet, a diet that focuses on natural, organic foods. (Note: Even when additives are derived from plant sources they can still be harmful.)
My perspective—that is, the patient’s perspective—makes this book unique and personal. Through my story, you will learn how I became an advocate for myself upon receiving a Crohn’s diagnosis. As the years went by and I developed a better understanding of my body and its healing, I became a resource for alternative therapies, and I want to further the mission of helping people balance their clinic treatments with Eastern medicine and healthy eating habits.
I remain quite healthy now, though not in full remission. I am dealing with active Crohn’s disease and ulcerative colitis by balancing a Western medical plan with a naturopathic treatment plan, an additive-free diet, along with acupuncture, massage, yoga and exercise (don’t forget getting enough sleep!).
I know what it is like to suffer from illness and want to help our readers and their caregivers regain wellness. We love to hear from readers, so please comment and let us know who you are doing and what works for you so we can share!
Dede’s friend, nutritionist Chris Ellis, is so knowledgeable and I’ve been bugging her to do a book with, too…. Here is a good overview of the Paleo diet.
Since I reported in my last article that I was a vegetarian some people may wonder why I would write about the other side of the diet spectrum, the currently popular Paleolithic Diet, which contains a significant amount of animal protein. I would respond by saying that every individual has specific dietary needs and not everyone biochemically or mentally feels at their optimal health being a vegetarian. I think everyone just needs to be aware of the choices and to do what feels best for their body physically, as well as what feels right for them philosophically. I would encourage individuals to be mindful of the impact their choices have on the environment and the earth too. In this article I am providing a little more insight into the Paleolithic Diet and hopefully that might help in exploring what type of eating plan works best for you or your family.
The Paleolithic Diet is a modern version of the diet that was followed by our ancestors many thousands of years ago. The diet was different wherever humans lived, depending on what animals also lived in the area for hunting and the availability of plants and seafood. The Paleolithic Diet was practiced prior to modern day agriculture and the domestication of animals. The diet consists of grass-fed animals such as beef and chicken, seafood, eggs, wild plants including vegetables (lots of root vegetables except potatoes), fruit, nuts (no peanuts), and seeds. The diet contained an ample supply of omega-3 fats mainly from the seafood, nuts, seeds, and the grass-fed animals since we had no surplus of corn and soybeans to feed our wild animals. Cereal grains are not a part of the diet and these include wheat, corn, millet, rice, barley, oats, sorghum, and rye. These grains were not available back then and they all need to be cooked in order to be consumed. The proponents of this diet believe that what humans ate back then is better suited genetically and biologically to our nutritional needs. Our human makeup is not coping well with the many changes in our present diet according to those who advocate for this diet and our bodies are not adapting well to the modern way of eating, specifically all the high calorie, highly processed foods. The root of many chronic health problems we face now, such as obesity, diabetes, heart disease, and cognitive disorders like depression and Alzheimer’s, are related to the diet most people follow in this country.
The changes in the modern diet include an increase of refined carbohydrates and cereal grains, a decrease in animal protein, a decrease in omega-3 fats, and an overabundance of sugary and salty foods such as candy, pretzels, chips, soda, etc. The modern American diet is comprised of approximately 50-60 percent carbohydrates, 15 percent protein, and 25 to 30 percent fat calories. The Paleolithic Diet, however, is comprised of approximately 25 to 30 percent protein, 40 percent carbohydrates, and 30 to 35 percent fat calories. The introduction of processed foods in the late 1800s definitely had an impact on the quality of our diet, and as our food supply became more industrialized the variety of crops and foods grown declined. But that is making a turnaround now, especially in Vermont, fortunately!
Humans are meant to eat a diversity of foods for optimal health but our diet today offers not only a wide variety of foods and ingredients but excess calories (sugar, unhealthy fats, corn products, etc.) far different from the hunters and gatherers regimen. We do not have to go far to get food, so very few calories are burned to “hunt or gather” our food. It is available on every corner depending on where you live, so long as you have the economic means to gather it.
So should we all eat the Paleolithic Diet? There are benefits to “eating Paleo” but our modern Paleolithic diet cannot duplicate the one followed by our ancestors. We are aware that there are benefits to a minimally processed diet and no matter what diet we choose we should strive to follow that. There are many good eating plans available (vegetarian, Mediterranean, Asian, etc.) and some may or may not contain meat and/or animal protein. It is best to consume animal protein from grass-fed animals (ideally with as little pesticides from their food as possible) with little or no use of drugs or hormones, safe wild seafood (not all fish is safe, as we know), and eggs, along with plentiful amounts of vegetables, seeds, nuts, and fruit—the basic Paleolithic Diet modified based on the dietary sources we have now that meet the guidelines. Choose an eating plan that you can follow that is optimum for your health and don’t forget to include an exercise component since that was an essential part of the Paleolithic lifestyle. We will all enjoy a longer healthier life if we follow some or all of the Paleolithic dietary guidelines!
~~~~
Questions? We’d love to hear from our readers and their own experiences with the Paleo Diet and IBD.
In the photo, from Living With Crohn’s & Colitis Book co-author, Dede Cummings, you can see the yummy roasted veggies that are perfect for the Paleo diet! The recipe is in my new cookbook, too!
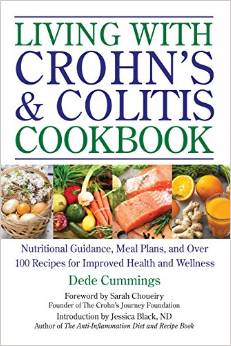 Our new cookbook is out and Dede would like to give away a free copy to the first two people who comment on this post — tell us a bit about yourself, are you a caregiver, do you have Crohn’s, or colitis, or IBS, or some other autoimmune disease? When you receive your book (send email in PM to dede@livingwithcrohnsandcolitisbook.com), please post a review on Amazon for us and we will be eternally grateful!
Our new cookbook is out and Dede would like to give away a free copy to the first two people who comment on this post — tell us a bit about yourself, are you a caregiver, do you have Crohn’s, or colitis, or IBS, or some other autoimmune disease? When you receive your book (send email in PM to dede@livingwithcrohnsandcolitisbook.com), please post a review on Amazon for us and we will be eternally grateful!
We are excited to share these gut-friendly recipes from the book and there is a long introduction about how to live with IBD and tips to help.
For the millions of people afflicted with irritable bowel disease (IBD), including Crohn’s and colitis, it can be a daily struggle to find nutritious meals that won’t aggravate symptoms or cause a flare-up. The Living with Crohn’s & Colitis Cookbook is your essential nutrition guide with over 100 recipes and meal plans expertly designed to improve daily functioning and help relieve symptoms of Crohn’s and colitis.
The Living with Crohn’s & Colitis Cookbook contains everything you need to plan your meals, balance your diet, and manage your symptoms, including:
• A guide to keeping a food journal
• Sample meal plans
• Tips for shopping for an IBD diet
• Gentle and nutritious recipes to help soothe flare-ups
…and much more!
The Living with Crohn’s & Colitis Cookbook features over 100 recipes, including Zucchini Buckwheat Banana Bread, Homemade Almond Milk, Dr. Lang’s Healing Soup, Garlic-Herbed Scallops, Coconut Curry Chicken over Brown Rice, Mushroom Risotto with Cashews and Parmesan, Crabapple Walnut Cake, and many more. The book also features Paleo recipes.
Enjoy these photos from our book!
Switching to a diet high in Omega-3s has been a major factor in my being in remission!
When I was first diagnosed with Crohn’s and colitis, I did not exactly jump into the fray of changing my diet and lifestyle… It took a few years! When you set out to try to change habits that are ingrained and also are associated with comfort (mother’s mac ‘n cheese anyone?), it takes time.

Wild-caught salmon follows the seasonal run of the Pacific Northwest. Photo courtesy of Central Mkt.
Now that I am on the other side of my twenty-year Crohn’s/colitis saga, I am in a place where I want to help others find their own way.
Once thing I have learned through my dietary study, is the fact that we need Omega-3 fatty acids in our diet daily—and not just if you are a Crohnie or uc-er. Every day.
I eat wild-caught salmon at least once a week, take flax seed ground up to aid in digestion and add fiber to my diet. I also take an Omega-3 supplement daily that really helps my arthritic joints (due to Crohn’s). I am healthy, fit and the doctors are surprised and how well I am, relying on diet, supplements and a holistic lifestyle.
Someone like me would normally be on autoimmune suppression drugs, but I do not want to do that to my body, and my choice was a wise one as I am incredibly healthy!
Omega-3 fatty acids are found also in walnuts, which I also eat every day. Other sources are the ALA (alpha-linolenic acid) Omega-3 fatty acids found in certain vegetable oils like soybeans, canola and flaxseed, as well as in green vegetables (kale, and more kale!, spinach, Brussels sprouts, and leafy greens). The other type of Omega-3 fatty acid is called EPA (eicosapentaenoic acid), and is present in salmon especially, as well as other types of fatty fish: Bluefish, mackerel, herring, tuna, anchovies and sardines are also excellent sources of omega-3s.
According to Dr. Frank Sacks, Professor of Cardiovascular Disease Prevention, Department of Nutrition, Harvard School of Public Health, you should have at least one serving of Omega-3 fatty acids in your diet daily.
In my upcoming cookbook, Living With Crohn’s & Colitis Cookbook: A Practical Guide to Creating Your Personal Diet Plan to Wellness (with an Introduction by Jessica Black, ND, and a Foreword by Sarah Choueiry, Crohn’s patient and founder of The Crohn’s Journey Foundation) due out in September (!), I have a few salmon recipes, and I’d like to share one now (quick and easy and great for summer dining—remember, if one of the foods, like apples, is a trigger food and hard to digest, substitute it or delete it from the recipe and adjust the mayo and seasonings accordingly)…. Enjoy!
Easy Salmon Salad
Ingredients:
2 cans wild boneless, skinless salmon
½ cup mayonnaise, organic
½ cup minced carrots
½ cup minced apples
¼ cup sweet relish, organic and sweetened naturally
Directions:
Mix all ingredients in a large bowl. Serve chilled with crackers, on a salad, or alone.
Source: http://www.hsph.harvard.edu/nutritionsource/omega-3/
….and I also want add a checklist for how to shop for the best salmon and how to cook and store the fish, as follows:
Wild-caught salmon (in photo) follows the seasonal run of the Pacific Northwest, and we strive to be first to market. According to the folks at Central Market, you should only buy from markets that buy fish from strictly regulated fisheries committed to sustainable practices and the guidelines set forth by the Marine Stewardship Council (MSC). The fish has been out of the water less than 48 hours prior to its arrival, flown in fresh several times a week and each piece is inspected.
Here are some tips from them to best enjoy your wild-caught salmon:
- Eat or freeze within 24 hours. Keep it in the refrigerator covered tightly in plastic wrap until you’re ready to cook it.
- Don’t rinse with water or the color will leach.
- If grilling, preheat grill to medium-high and grease it well with olive or grapeseed oil. Place the salmon on the grill, meat side down, and cook for 3 to 4 minutes, depending on thickness of the fillet. Flip over and cook 3 to 4 minutes more, skin side down. Also try it with a cedar plank. Sear with meat side down, then place skin side down on cedar plank and close the grill to infuse that cedar-smoked flavor.
- If using a cast-iron skillet, heat it until almost smoking and sear 2 to 3 minutes on each side. Pull it off the heat and let it continue to cook in the skillet until desired doneness.
- Salmon is done when it starts to flake, and it tastes best with a medium center.
Now that you know how to store and prep your salmon—enjoy! You can also pre-order my cookbook right here at your local, independent bookstore, and Sarah Choueiry and I are really excited to introduce you to a ton of great and easy recipes!
Happy Almost Summer!
I found this photo this morning, when I was remembering how scared I was going in for surgery for a bowel resection due to a serious, three-week, blockage of my small intestine from complications of Crohn’s disease.
I only weighed 117 pounds in this photo, taken with my son’s college roommate, Justin, two days before my operation in 2006. I was so skinny and malnourished, it’s hard to believe now that I am over twenty pounds heavier! I also found my husband’s post on my CaringBridge site (which still exists under “DedeCummings”), and I want to tell all my readers and followers of this blog, that you should never give up hope!
Written May 22, 2006 8:35pm
Hi all–
The news from Hanover is very good: Dede was in surgery from about 9:30-noon, and awoke (in a manner of speaking) about an hour later. She had a good grip on the button of her morphine pump, and smiled beatifically every time she heard its answering “beep.”Dr. Henriques took out approx. 5 inches of her small intestine, of which 5 cm had severe scarring and the rest was worn out, and about the same length of large intestine, which had been scarred by a fistula (an “abnormal passage” connecting the two, resulting from her disease/scarring). The doctor held up his index fingers like a fisherman describing his catch when describing all of this.
He also took out her appendix while he was in there, so we’ll have no access to supplementary information about her internal organs in the future. (Sorry: lame book joke…) Her gall bladder looks fine, just for the record.
He expects her to be in the hospital for only a few days, so she could get home as soon as Thursday. She has already gotten out of bed, taken a few steps, and sat up for a while.
By tomorrow she’ll be treated to smoothies and milkshakes, and can eat some solid food by the end of the week–Dr. Henriques predicts that she’ll be voracious by that point.
Thanks for all of your lovely notes and positive thoughts; I’ll be able to get my computer online in her room tomorrow, so keep ’em coming.























