Dede’s friend, nutritionist Chris Ellis, is so knowledgeable and I’ve been bugging her to do a book with, too…. Here is a good overview of the Paleo diet.
Since I reported in my last article that I was a vegetarian some people may wonder why I would write about the other side of the diet spectrum, the currently popular Paleolithic Diet, which contains a significant amount of animal protein. I would respond by saying that every individual has specific dietary needs and not everyone biochemically or mentally feels at their optimal health being a vegetarian. I think everyone just needs to be aware of the choices and to do what feels best for their body physically, as well as what feels right for them philosophically. I would encourage individuals to be mindful of the impact their choices have on the environment and the earth too. In this article I am providing a little more insight into the Paleolithic Diet and hopefully that might help in exploring what type of eating plan works best for you or your family.
The Paleolithic Diet is a modern version of the diet that was followed by our ancestors many thousands of years ago. The diet was different wherever humans lived, depending on what animals also lived in the area for hunting and the availability of plants and seafood. The Paleolithic Diet was practiced prior to modern day agriculture and the domestication of animals. The diet consists of grass-fed animals such as beef and chicken, seafood, eggs, wild plants including vegetables (lots of root vegetables except potatoes), fruit, nuts (no peanuts), and seeds. The diet contained an ample supply of omega-3 fats mainly from the seafood, nuts, seeds, and the grass-fed animals since we had no surplus of corn and soybeans to feed our wild animals. Cereal grains are not a part of the diet and these include wheat, corn, millet, rice, barley, oats, sorghum, and rye. These grains were not available back then and they all need to be cooked in order to be consumed. The proponents of this diet believe that what humans ate back then is better suited genetically and biologically to our nutritional needs. Our human makeup is not coping well with the many changes in our present diet according to those who advocate for this diet and our bodies are not adapting well to the modern way of eating, specifically all the high calorie, highly processed foods. The root of many chronic health problems we face now, such as obesity, diabetes, heart disease, and cognitive disorders like depression and Alzheimer’s, are related to the diet most people follow in this country.
The changes in the modern diet include an increase of refined carbohydrates and cereal grains, a decrease in animal protein, a decrease in omega-3 fats, and an overabundance of sugary and salty foods such as candy, pretzels, chips, soda, etc. The modern American diet is comprised of approximately 50-60 percent carbohydrates, 15 percent protein, and 25 to 30 percent fat calories. The Paleolithic Diet, however, is comprised of approximately 25 to 30 percent protein, 40 percent carbohydrates, and 30 to 35 percent fat calories. The introduction of processed foods in the late 1800s definitely had an impact on the quality of our diet, and as our food supply became more industrialized the variety of crops and foods grown declined. But that is making a turnaround now, especially in Vermont, fortunately!
Humans are meant to eat a diversity of foods for optimal health but our diet today offers not only a wide variety of foods and ingredients but excess calories (sugar, unhealthy fats, corn products, etc.) far different from the hunters and gatherers regimen. We do not have to go far to get food, so very few calories are burned to “hunt or gather” our food. It is available on every corner depending on where you live, so long as you have the economic means to gather it.
So should we all eat the Paleolithic Diet? There are benefits to “eating Paleo” but our modern Paleolithic diet cannot duplicate the one followed by our ancestors. We are aware that there are benefits to a minimally processed diet and no matter what diet we choose we should strive to follow that. There are many good eating plans available (vegetarian, Mediterranean, Asian, etc.) and some may or may not contain meat and/or animal protein. It is best to consume animal protein from grass-fed animals (ideally with as little pesticides from their food as possible) with little or no use of drugs or hormones, safe wild seafood (not all fish is safe, as we know), and eggs, along with plentiful amounts of vegetables, seeds, nuts, and fruit—the basic Paleolithic Diet modified based on the dietary sources we have now that meet the guidelines. Choose an eating plan that you can follow that is optimum for your health and don’t forget to include an exercise component since that was an essential part of the Paleolithic lifestyle. We will all enjoy a longer healthier life if we follow some or all of the Paleolithic dietary guidelines!
~~~~
Questions? We’d love to hear from our readers and their own experiences with the Paleo Diet and IBD.
In the photo, from Living With Crohn’s & Colitis Book co-author, Dede Cummings, you can see the yummy roasted veggies that are perfect for the Paleo diet! The recipe is in my new cookbook, too!
Switching to a diet high in Omega-3s has been a major factor in my being in remission!
When I was first diagnosed with Crohn’s and colitis, I did not exactly jump into the fray of changing my diet and lifestyle… It took a few years! When you set out to try to change habits that are ingrained and also are associated with comfort (mother’s mac ‘n cheese anyone?), it takes time.

Wild-caught salmon follows the seasonal run of the Pacific Northwest. Photo courtesy of Central Mkt.
Now that I am on the other side of my twenty-year Crohn’s/colitis saga, I am in a place where I want to help others find their own way.
Once thing I have learned through my dietary study, is the fact that we need Omega-3 fatty acids in our diet daily—and not just if you are a Crohnie or uc-er. Every day.
I eat wild-caught salmon at least once a week, take flax seed ground up to aid in digestion and add fiber to my diet. I also take an Omega-3 supplement daily that really helps my arthritic joints (due to Crohn’s). I am healthy, fit and the doctors are surprised and how well I am, relying on diet, supplements and a holistic lifestyle.
Someone like me would normally be on autoimmune suppression drugs, but I do not want to do that to my body, and my choice was a wise one as I am incredibly healthy!
Omega-3 fatty acids are found also in walnuts, which I also eat every day. Other sources are the ALA (alpha-linolenic acid) Omega-3 fatty acids found in certain vegetable oils like soybeans, canola and flaxseed, as well as in green vegetables (kale, and more kale!, spinach, Brussels sprouts, and leafy greens). The other type of Omega-3 fatty acid is called EPA (eicosapentaenoic acid), and is present in salmon especially, as well as other types of fatty fish: Bluefish, mackerel, herring, tuna, anchovies and sardines are also excellent sources of omega-3s.
According to Dr. Frank Sacks, Professor of Cardiovascular Disease Prevention, Department of Nutrition, Harvard School of Public Health, you should have at least one serving of Omega-3 fatty acids in your diet daily.
In my upcoming cookbook, Living With Crohn’s & Colitis Cookbook: A Practical Guide to Creating Your Personal Diet Plan to Wellness (with an Introduction by Jessica Black, ND, and a Foreword by Sarah Choueiry, Crohn’s patient and founder of The Crohn’s Journey Foundation) due out in September (!), I have a few salmon recipes, and I’d like to share one now (quick and easy and great for summer dining—remember, if one of the foods, like apples, is a trigger food and hard to digest, substitute it or delete it from the recipe and adjust the mayo and seasonings accordingly)…. Enjoy!
Easy Salmon Salad
Ingredients:
2 cans wild boneless, skinless salmon
½ cup mayonnaise, organic
½ cup minced carrots
½ cup minced apples
¼ cup sweet relish, organic and sweetened naturally
Directions:
Mix all ingredients in a large bowl. Serve chilled with crackers, on a salad, or alone.
Source: http://www.hsph.harvard.edu/nutritionsource/omega-3/
….and I also want add a checklist for how to shop for the best salmon and how to cook and store the fish, as follows:
Wild-caught salmon (in photo) follows the seasonal run of the Pacific Northwest, and we strive to be first to market. According to the folks at Central Market, you should only buy from markets that buy fish from strictly regulated fisheries committed to sustainable practices and the guidelines set forth by the Marine Stewardship Council (MSC). The fish has been out of the water less than 48 hours prior to its arrival, flown in fresh several times a week and each piece is inspected.
Here are some tips from them to best enjoy your wild-caught salmon:
- Eat or freeze within 24 hours. Keep it in the refrigerator covered tightly in plastic wrap until you’re ready to cook it.
- Don’t rinse with water or the color will leach.
- If grilling, preheat grill to medium-high and grease it well with olive or grapeseed oil. Place the salmon on the grill, meat side down, and cook for 3 to 4 minutes, depending on thickness of the fillet. Flip over and cook 3 to 4 minutes more, skin side down. Also try it with a cedar plank. Sear with meat side down, then place skin side down on cedar plank and close the grill to infuse that cedar-smoked flavor.
- If using a cast-iron skillet, heat it until almost smoking and sear 2 to 3 minutes on each side. Pull it off the heat and let it continue to cook in the skillet until desired doneness.
- Salmon is done when it starts to flake, and it tastes best with a medium center.
Now that you know how to store and prep your salmon—enjoy! You can also pre-order my cookbook right here at your local, independent bookstore, and Sarah Choueiry and I are really excited to introduce you to a ton of great and easy recipes!
Happy Almost Summer!
In some human diseases, the wrong mix of bacteria seems to be the trouble.
I recently discovered a new blog that is specifically for Chronic Fatigue Syndrome and Fibromyalgia. It is called Health Rising and the link is below.
There are articles that explore gut health and microbiota by Ken Lassesen, that really explain the importance on overall homeostasis for everyone, whether you have Crohn’s, colitis, IBS, IBD, Celiac, etc.
I am on a strict diet of no dairy, no grains, no sugar. Supplements include probiotics and turmeric. I am really healthy and haven’t had symptoms for almost eight years! I did have a partial bowel resection, in 2006, that changed my life and set me on a path toward wellness— that is when I wrote my book because I was disillusioned by the recommendations of my GI doctors who said I should take heavy-duty, autoimmune-suppressing drugs.
Read more: Bacterial Resistance, Infection and Chronic Fatigue Syndrome: Fighting Infections Pt. I http://www.cortjohnson.org/blog/2014/03/26/bacterial-resistance-infection-chronic-fatigue-syndrome-fighting-infections-pt-1/
~~~
~
In some human diseases, the wrong mix of bacteria seems to be the trouble, Part 2.
A recent NPR story on gut bacteria and Crohn’s disease really impressed me, so I want to share it in its entirety here on my blog!
Mix Of Gut Microbes May Play Role In Crohn’s Disease
The particular assortment of microbes in the digestive system may be an important factor in the inflammatory bowel condition known as Crohn’s disease.
Research involving more than 1,500 patients found that people with Crohn’s disease had less diverse populations of gut microbes.
“[This] basically for the first time identifies what might be the bacterial changes in patients with Crohn’s disease,” says Ramnik Xavier, of Masssachusetts General Hospital in Boston, who led the work.
More than a million Americans suffer from Crohn’s, which seems to start when an overreactive immune system causes abdominal pain, diarrhea, bleeding, weight loss and other symptoms. Many patients have to take powerful steroids (which can have serious side-effects), and some have parts of the digestive tract surgically removed.
Mounting evidence has suggested that microbes living in the gut might contribute to the problem. So Xavier and his colleagues compared the species of bacteria in more than 447 Crohn’s patients to the mix of microbes in more than 221 healthy people.
In their paper published in the journal Cell, Host and Microbe, the researchers detailed the clear difference they discovered: The patients with Crohn’s seemed to have too many of the sorts of bacteria that rile immune systems.
In addition to having less diversity in their gut microbes, Xavier says, the Crohn’s patients had fewer bacteria that have been associated with reduced inflammation and more bacteria associated with increased inflammation. (The findings were confirmed in 800 Crohn’s patients from other studies.)
Interestingly, children whose doctors had tried to treat their Crohn’s symptoms with antibiotics before they were properly diagnosed had a mix of microbes that was the most out of whack.
“We may have to revisit the use of antibiotics in [these] patients with early-onset Crohn’s disease,” Xavier says.
Instead, doctors might eventually do better to identify and prescribe treatments that mimic the helpful bacteria, he says, along with foods or other pharmaceutical agents that reduce or counteract the harmful bacteria.
“There’s the possibility that we might be able to identify [some] sort of super-probiotics that might be able to correct the gut back to the healthy state,” Xavier says.
UCLA pathologist Jonathan Braun, who studies microbial ecology, says the paper offers important first insights into illnesses beyond Crohn’s. “Other diseases are thought to be driven at least in part by bacteria,” he says, such as some inflammatory and autoimmune disorders. Bacteria may also be involved in obesity.
Humans should work harder to understand bacteria, Braun says, “and live with them when they’re helping us, or get them to serve us better when they are causing harm.”
~
Good for the media to pick up in the importance of balance in the flora and fauna of the gut—remember, everyone is different and there is no know cure for Crohn’s (for UC, the large colon can be removed, putting the patient in remission, but that is not the case for Crohn’s unfortunately).
So, with Spring on the way, now is the time to set some goals for health: sign up for Team Challenge with the Crohn’s and Colitis Foundation of America, walk 3 miles a day (get your heart rate up by walking up hills), do yoga/meditate, get lots of sleep, make an appointment with a naturopath, too. Spring brings with it hope for new life (and here in Vermont, lots of mud!).
Happy Holidays from Dede & Jessica at Living With Crohn’s & Colitis!
This plan was developed as a guide for generating a treatment regimen. Just as each individual is unique, so too is their road to wellness. This 3-month plan is meant to be used loosely, so you should feel free to adjust each step as needed for your own recovery. Please consult your physician when beginning this program, and continue to visit your established team of specialists (naturopath, gastroenterologist, etc.) so that they can help you monitor your progress and make any necessary adjustments to the program.
As discussed in our book—and is a good idea to read the book before beginning this plan—treatments and lifestyle changes can occur in any order, but here we have provided a plan that will slowly and gently move you through your digestive problems and into wellness. Most patients will feel some positive changes as they progress through this 3-month plan and some patients may even become symptom-free.
The most important aspect of this step-by-step process for building health is that we are creating a foundation for wellness and building upon it, rather than trying to overwhelm the body by incorporating all changes at once. Taking new strides each week helps to keep you focused and motivated through the entire process. We know that change can be overwhelming, which is why we’ve created this program so that it can also be slowed down even further to incorporate new changes every 3 weeks and can be specifically tailored to your individual needs.
NOTE: All severe conditions and the need for surgery must be ruled out by your physician prior to starting this program. If initial acute symptoms are severe, they must be treated either with natural medicine or pharmaceutical medicines to provide relief while working on the underlying imbalances.
NOTE: Stress is a precursor to disease and flare-ups. If you are a parent of a child with IBD, or a patient or caregiver, try to help keep the holidays as stress-free as possible! (Easy for me to write this, as I woke up at 3:00 a.m. worrying about buying presents …. and planning a party! Yikes. But I am off to walk 4 miles this morning AND DO YOGA AND MEDITATE!!!
Weeks 1–2:
1. See the change and believe in the change! Visualize optimal colon health daily. See yourself happy, active, and vibrant in your mind.
2. Proper Mealtime Habits—eat slowly, and take your time preparing, shopping, and don’t overeat, or try new foods during the holidays!
3. Remove major dietary causes of inflammation—keep a food journal, and stay away from trigger foods!
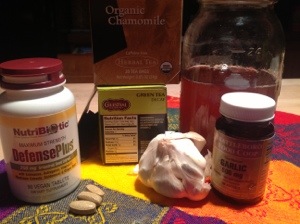
4. Add only one supplement or herbal medicine, whichever best suits you. This may be an acute remedy for diarrhea, acidophilus, or any other supportive medicine—for example. I just bought a new supplement—turmeric—because I ran out.
5. Herbal teas: pick one of the teas that best fit your needs and drink daily. I choose Perppermint! Also Chamomile is a good stress reducer. Add honey for sweetening (NO SUGAR AT ALL!)
Weeks 3–4:
1. Continue previous points.
2. Add an additional supplement or herbal medicine—talk to your doctor or naturopath about Vitamin D, or Omega 3.
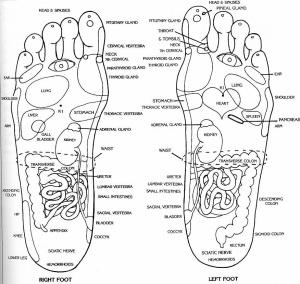 3. Begin the Tapping for Energy technique (in our book) or daily acupressure. Dede likes to massage her feet before bed, using a nice mix of moisturizer and sesame or apricot oil. It is amazing how much stress in in our feet and the acupressure points relate to organs in the body. It is a great routine to press gently on some of these points — the chart shows you were the bowel area is (also liver point is important to gently press).
3. Begin the Tapping for Energy technique (in our book) or daily acupressure. Dede likes to massage her feet before bed, using a nice mix of moisturizer and sesame or apricot oil. It is amazing how much stress in in our feet and the acupressure points relate to organs in the body. It is a great routine to press gently on some of these points — the chart shows you were the bowel area is (also liver point is important to gently press).
4. Experiment with adding more anti-inflammatory foods and spices into your diet. Last night, I made a fish curry with garnishes of bananas, raisins, chopped apples . . . yum!
Message me if you want the recipe. It was mild, not too spicy, and used Haddock filet.
Weeks 5–6:
1. Continue previous points.
2. Add an additional supplement or herbal medicine. I take grape seed extract when I feel a cold or flu coming on. Try a warm bath at night with lavender oil.
3. Begin to incorporate movement/exercise. Do this at least 3 times per week, but daily possible. This is VERY important…start slowly, but try every day. Begin with your mind—just change the way you think about exercise (like when you get busy at work or with life, don’t eliminate it!).
Weeks 7–8:
1. Continue previous points.
2. Incorporate daily nutritional powders into your diet such as spirulina, kelp, green tea, or acai powder—try these sparingly at first, and make sure nothing irritates (Dede does not use spiraling, but kelp and green tea really help keep inflammation at bay. An excellent overall nutritional supplement, but use the best brand and tell your doctor. Here is a nice article from Dr. Oz on acai powder. Dede has acupuncture once a month-another great thing to introduce—if it is too expense, find a “community-supported acupuncture” place to go, like a clinic. Dede’s acupuncturist gives her a discount ($55 per 1 hour session!) because she has a sliding scale. Acupuncture really helps!
3. Add an additional supplement, if needed. PROBIOTICS ARE GREAT, according to Dede, who takes 1/4 teaspoon of powder every day. Again, buy from Naturopath, or Metagenics is a good company. Dede uses “Synergy” brand, all flora.
Weeks 9–10:
1. Continue previous points.
2. Add an additional supplement if needed. Talk to your doctor about your magnesium/calcium levels—Dede takes a mag-citrate because she doesn’t have dairy in her diet. Plus, if you have been on steroids for treatment, you want to be sure your bone health/density is good, so it would be wise to talk to your doctor about having a test.
3. Incorporate mental and emotional support. This may be needed sooner in some individuals suffering from anxiety and depression contributing to their illness. Dede swears by “Talk Therapy,” and goes 2x a month. She tells her therapist everything about dealing with her disease, work, relationships, boundaries, stress, etc. THE BEST!
Weeks 11–12:
1. Continue previous points.
2. Add an additional supplement if still needing more support. Talk to your naturopath. Your electrolytes need to be balanced. Dede makes homemade chicken soup broth 2x a month. Dede loves being on a Paleo-like diet! NO SUGAR, NO GRAIN (can use Almond and Coconut flours), NO DAIRY!! This is the best! Use Almond mile, eat eggs and organic animal proteins (local chicken is good, beef—but make sure it is antibiotic-free and free range)
3. Incorporate colon hydrotherapy (castor oil packs 5 days per week or constitutional hydrotherapy treatments — details are in our book, along with tons of other lifestyle information! Dede loves her castor oil pack-when her abdomen is sore, she lies down with the pack and a heating pad, and reads, or meditates, or sleeps. Pain goes away!.
HAPPY HOLIDAYS!
Enjoy a stress-free New Years, and look forward to 2014! Remember, a positive attitude improves disease outcome, so “THINK POSITIVE!”
Since it is almost Thanksgiving, I thought I would write a post to wish everyone a happy, stress-free holiday, and try to help those with IBS, Crohn’s, and UC who may need some encouragement and advice.
We all know holidays can bring on the stress-inducing behaviors and hormones that cause internal signals to flare up in the body. When I was at the Mayo Clinic a few (short) months ago, I learned so much about controlling stress—make stress-reducing activities a priority, starting today, and leading up through the holiday season.
Your lifestyle structure is even more important here: daily exercise, gentle yoga, meditation, sleep, etc. Schedule appointments with professionals to help you lessen stress in your life: a talk therapist, acupuncture, massage (gift cards are good holiday presents for those you love!), etc. Do what makes you feel good about yourself AND relax! (I went to the salon yesterday for hair color!)
Tryptophan is one of the 10 essential amino acids that the body uses to synthesize the proteins it needs. It’s well-known for its role in the production of nervous system messengers, especially those related to relaxation, restfulness, and sleep.
I am now aware why I love turkey so much—I sometimes even crave it. I always feel more relaxed after I eat turkey, and this may explain why….There are many researchers who study the way tryptophan manufactures serotonin, a neurotransmitter that is found—guess where?—in the intestinal tract. Just about 90% of the body’s serotonin is actually found in the gut, so my gut tells me to eat it, and I am not even a biochemist!
Tryptophan has the ability to raise serotonin levels, too! Wow, who knew this? I love the fact that I can eat turkey and sample other holiday foods like nuts, seeds, bananas, pumpkins, squash, sweet potatoes, green beans with almonds, pearl onions (those sweet little ones, not the canned and creamed kind!) WITHOUT having a flare up. Also (again, who knew?!), Tryptophan also boosts the production of B3, and since I had a partial bowel resection in 2006, I need to keep track of my B vitamins (especially since my terminal ileum is completely gone, I have lost the capacity to fully absorb vitamin B12).
Everything I eat is sourced, and mostly bought from local farms. It is not that hard to do. For instance, our turkey is a Vermont-raised, free running turkey, and I picked it up yesterday from our local food coop. Potatoes are from here, also butternut squash, apples, pumpkins—are all from Vermont; cranberries are organic and from Cape Cod. I will be baking apples, too—delicious and easy. Some of us cannot eat nuts or cranberries, so avoid, but there is plenty to choose from!
Here are some tips: drink water before your meal to fill you up so you don’t overeat, take small portions, walk after the meal. If you have an ostomy, take extra supplies and a change of clothes to your hosts’ party. If you avoid sugar and alcohol, you will be less likely to flare up; also don’t try ANY food that is not on your list (remember the food journal from the book!).
On Wednesday/tomorrow, I will make some pies to drop off at our local Thanksgiving Day dinner for those less fortunate in our area—Don’t forget to do something to help someone else in need this week, and after. With all the holidays upon us, plan some special time each week to volunteer (soup kitchen, helping those who have been in a house fire, helping veterans, etc.). Thanksgiving was set as the fourth Thursday in November. This year, something amazing and historic has happened: After sundown on the second of Hanukkah’s eight days, we will also celebrate Thanksgiving. If you are Jewish, there is an even busier holiday!
I will post some recipes on my Facebook page! Be well, and breathe … A bit of dietary research unravels mysteries of cravings from this writer with uc/Crohn’s disease….Happy Thanksgiving & holidays everyone!
Good day to my fellow Crohnnie’s and UC-ers,
Holidays are fun—remember that!!! In the spirit of our favorite holiday when you have IBD, we are gearing up for a gluten-free, dairy-free, sugar-free, AND grain-free Thanksgiving!!! Yahoo! Can’t wait. Here is what we can eat: TURKEY!!! The best comfort food on earth (with lots of tryptophan in it that makes us feel good), sweet potatoes (yams) that are steamed and mashed with olive oil and a bit of melted canola butter on top, small sweet onions with canola butter, steamed carrots, cranberry sauce (unsweetened), as long as you can tolerate cranberries. Don’t try ANY new food over any holiday. If you go to a potluck, don’t eat, or bring your own food …. Remember to stay positive, get a lot of rest and exercise every day to clear your head. Start meditation, and volunteer at a local Thanksgiving Day dinner (I’ll be making some gluten-free dishes to bring to my town’s open dinner as a donation)….
Take care of yourself! Give back to others, and you will have a perfect holiday!
Here are some more of Dede’s “Living-with-Crohn’s & Colitis” TIPS—
Probiotic & Diet
For PROBIOTICS, look for a pure brand with a 50/50 blend of bifidobacterium and lactobacillus acidophilus. Perhaps you can find this brand: Metagenics, Ultra Flora “Synergy.” Take once a day, with or without food (depends on how you tolerate it). Keep that food journal, and note down any stress in your life, daily exercise, everything you eat. Don’t eat fried or spicy food—keep track, and eat small frequent meals. I have a really OCD technique: breakfast begins with tea and a dash of milk (the ONLY dairy I eat, and my ONE treat ;)), then add a bit of honey (again, buy in bulk and a pure brand). Cold cereal of almond milk mixed with bananas and cut-up melon (add nuts and raisins IF you can tolerate). Snack is peanut butter on carrots.
CHEW EVERYTHING really well!
Drink TONS of water with fresh lemon squeezed into it.
Drink TONS of herbal teas…I like peppermint
Lunch is tuna or chicken salad (use pure fresh, virgin, olive oil!), maybe chick pea humus and a handful of almonds on the side; snack is applesauce and peanut butter. Dinner is a grilled local beef/organic hamburger with steamed zucchini. No grain, no sugar, no dairy. I eat ALL the time and feel great on this diet. I don’t even crave sugar!
Good luck and stay positive. YOU CAN DO THIS!
RX, Flare—Where to begin…. Here are some lifestyle tips, from Dede, who has been in remission from Crohns for almost eight years…. Do not despair.
“There is a saying in Tibetan, ‘Tragedy should be utilized as a source of strength.’
No matter what sort of difficulties, how painful experience is, if we lose our hope, that’s our real disaster.”
—The Dalai Lama
Take control: hydrate, sleep, exercise, yoga meditation, daily…
Walk 1-4 miles per day
Sleep at least 8 hours per night (take powdered magnesium bicarbonate—Dede likes “Natural Vitality’s Natural CALM in the Raspberry-Lemon flavor, drink fresh-squeezed lemon-lime-flavored water all day long (carry glass water bottle with you, and the new ones are encased in non-breakable plastic or rubber)
Drink herbal teas—Chamomile, dandelion root, peppermint— and also Green Tea that has caffeine, but also comes in decaf.
Movement & Meditation
Start a gentle yoga DvD (Rodney Yee’s a.m. Yoga is wonderful), and set up a “yoga studio” in your house or apartment somewhere (mine is in the basement with an old TV, but I have made it my own with a little table and a small wooden Buddha, candles—it is peaceful and my own space).
This yoga will lead to guided meditation. Even 5-10 minutes a day improves patient outcomes! A local class or “sangha,” is a nice way to learn to meditate.
Watch Your Diet
Once you get in tune with your body, you can start to really tell if certain foods make you begin to flare and you can back off immediately and note in your journal to keep track.
Keep a list of safe foods, foods to avoid.
Body Care—It Pays to Be Beautiful!
Use essential oils to sniff daily. I like lavender oil in my bath, eucalyptus oil in the shower
Massage your feet every night before you go to bed. Use a nice moisture lotion (with lavender, if you like it), and I add organic apricot or sesame oil to make it thicker.
Take some “Natural Calm” magnesium powder each night in a hot glass of water before you go to bed… You will sleep better!
Massage the back of your neck—press with acupressure in the “still point” at the base of your skull—get a friend, or spouse, to help.
Speaking of….ASK FOR HELP! Don’t do what I did, which was to lie in bed and retreat from the world for days at a time…the only trip to the bathroom for a journey…. Ask for help—on Facebook, or pick up the phone.
See a therapist, once a month, or join a group for IBD, Crohn’s, colitis, or autoimmune disease.
Volunteer at a soup kitchen or homeless shelter, or environmental action group…. Altruistic behavior helps you to let go of stress.
Last, but not least, LAUGH every day! Watch the stupid pet videos… Or this goofy video my friend, Dodie, sent me this morning… She is going through cancer treatment, and she is very brave and a wonderful friend, who retains a sense of humor!
~~~~~~~
;))
It is amazing how much a positive attitude can help. In our book, there is a section when I am despairing and a doctor comes and sits with me and holds my hand—no kidding! He said, “Think positive.” Well, on that note, I want to write a post today about that and helping the body adjust to the changing season and of course living with IBD in general. I also want to share the news that I am writing a cookbook, called Living with Crohn’s & Colitis Cookbook (good title, too!)…my publisher is the wonderful Hatherleigh Press, which is distributed by Random House. I couldn’t ask for a better team! Publisher, Andrew Flach believed in this book from the very start, associate publisher, Ryan Tumanbing is always there when I need things, and my editor, Anna Krusinski is da Bomb!
My book with Jessie is a good overview and a way to understand how the body chemistry and immune response works. I am not denying the benefits of medication, but we do offer an alternative, and if you are someone who has to stay on meds, you can do both—no matter what, it is important to keep the body tuned and in a balanced state of homeostasis.
Getting a full work up from a medical professional is the first step—go to a specialist at a GI clinic (Dartmouth is the best in my area), and have a colonoscopy, blood work (really important as many patients are anemic due to blood loss, or low in B-12 as in my case), a physical exam (a patient will no doubt be embarrassed by this like I was, but this is a very important exam because the doctors can determine a lot when they examine the anus and rectum, and palpitate the abdomen—they could feel the mass in my case), and what is called enterography: a MRI or CAT scan (I don’t recommend CAT scans too frequently for younger people) will reveal areas of disease inflammation.
Crohn’s typically presents in the lower right abdominal quadrant (often confused with the appendix!) of the small intestine, but it can strike anywhere from the mouth to the anus. Colitis presents throughout the large intestine only. Crohn’s really cannot be cured, and has a tendency to skip to infect the next section of the bowel even after the diseased section has been removed (as in my case). Colitis can be cured through surgery if nothing else (drug therapy or naturopathic-holistic-alternative) works. They take out the large colon, and connect the stomach-duodenum-small bowel through a J-pouch internally, or an external ostomy bag. Not a great thing for anyone to have an ostomy bag; however I have met many people with colitis who don’t mind the bag at all, and love the fact that they are pain-free.
The Crohn’s & Colitis Foundation of America is the best organization! I love everyone there, and run in their half marathons with Team Challenge to help raise money for research; plus it is a community of fellow patients, young and old, and we are a surprisingly close-knit group. Join, and sign up for a walk and a support group (they even have a new college group!) as soon as you can.
The other thing to do, is have a poop sample tested (this is no fun, but can tell a lot—bacterial infections, or something called C-Diff). In addition to going to a GI clinic, make an appointment for a work-up with a recommended naturopath, a trained naturopathic physician with a four-year degree from a well-known college (Bastyr University, for example) and get right in there for a checkup and a plan of action. My naturopath did allergy testing to see if there were specific foods (most common culprits are wheat and dairy), that I needed to eliminate, and she ordered an endocrine hormone test to see if I may have had a hormone imbalance.
I also give a lot of credit to my acupuncturist who is trained in Chinese medicine, and I go once a month. It is all in our book, but make sure you stay on top of the disease and get regular check ups with your medical doctor to rule out any other complications. I had a dangerous abdominal fistula, that didn’t show up on the CAT scan and was attaching itself to another organ—sorry to bring in the drama, but IBD (Inflammatory Bowel Disease) can be life threatening. No question, it is vitally important to be proactive, especially as a parent.
My weight was so low, I was dangerously thin—ironic, because our society places such status on being thin! I am now a healthy 140 pounds, and I work hard every day to stay healthy. Once I get busy with work, and let things slide, I start to feel run down… I can tell right away! Being in tune with your body is very helpful—keeping a food and daily journal, getting some good private counseling, and doing stress reduction exercises (Tai Chi or yoga) daily is also a big part of managing the disease.
I think I have covered the basic tenets of my book with Dr. Jessie. Oh, one more thing, join the online groups— http://www.ihaveuc.com, and The Crohn’s Journey Foundation for starters, also Intense Intestines, Girls With Guts, the Crohn’s Forum, Healing Well, and others. We are a strong and awesome group—always there to support each other! Let’s face it, the doctors are so busy, they can’t spend and hour with each patient, and it is the patients themselves who are doing great research and offering support. If a doctor tells you stress or diet have nothing to do with IBD, find another doctor! Oh, and second opinions are a good plan as well.
I have eliminated SUGAR, and ALL grains from my diet and ALL dairy. It is awesome! I feel so much better… I eat baked chicken or grilled fish, locally-raised, antibiotic-free, grass-fed hamburger steak once in a while when my body craves red meat, all served with yummy vegetables on the side and tons of fruit and nuts and eggs… I take extra calcium-magnesium, along with daily probiotics, turmeric, Omega 3, Vitamin D, herbal adrenal support, extra vitamin C, and a good multi-vitamin (I buy only organic food and supplements—it’s more expensive, but then I don’t spend a lot of money on clothes and makeup!).
So that is the basic overview—I am always there for my readers, and want to offer as much support as possible!
Oh, this just in, Dede will be on The Doctor Oz show this coming Monday, October 14th, in a spot on how common bloating is. They found me through the Crohn’s-Colitis book on “Help a Reporter Ou”t (HARO), and asked me to show how hard it is to buckle my jeans when I am bloated, which is what “used to happen” when I ate too much dairy or wheat…now, I don’t have bloating much AT ALL! Watch the segment if you want a laugh 😉 as “laughter is the best medicine.” I don’t mind embarrassing myself to help others…
Be well, and take care of yourself… don’t be afraid to ask for help!
Dede
Below, you can see some recent dinners… My husband and I have a grill we use a lot, and here you can see grilled marinated swordfish (fresh ginger root, white wine, wheat-free tamari, lime, and a dash of brown sugar for the marinade and let sit for a half hour before grilling) with grilled garden-fresh small eggplants (some people may have trouble with seeds…always introduce new foods slowly and note the reaction by your body in your journal right away….like I tried polenta this summer….noooooo! Not good for me, but may not bother someone else—we are all different!), and baked chicken with a sesame glaze (it was so good!) and steamed broccoli.
On July 21st, Brattleboro, Vermont resident, Dede Cummings, ran the Napa-to-Sonoma Wine Country Half Marathon with Team Challenge New England to raise funds for the Crohn’s & Colitis Foundation of America (www.CCFA.org). This was her second Half Marathon with Team New England, and there were over 3,500 runners competing, with 672 from the CCFA.
Cummings ran to raise research funds for the CCFA, whose mission is to find a cure for Inflammatory Bowel Diseases and improve the quality of life of the 1.5 million American adults and children who suffer everyday, with a time of 2-1/2 hours and she placed in the middle of the racers on race day.
Since she is from Vermont, she ran with Team Challenge from New England, and the group wore “Boston Strong” T-shirts. Team New England raised the most money of all the teams, over $400,000. The total money raised for the event was over $2.4 million dollars of which 80% goes to research. There were teams from across the United States, running to raise money for the Crohn’s & Colitis Foundation of America.
Cummings also ran for Ryan McMahon, a former team challenge runner who was injured in the Boston bombing. She is now part of a group called Run for Boston (#runforboston), which is motivated to raise awareness for running as well as for the increase in inflammatory bowel disease worldwide.
According to Cummings:
At mile 12, we turned right and entered the small city of Sonoma. At this point people were lining the street, and urging us on, which was great. Both of my calves cramped up pretty badly, and I was kind of nervous. I could see the finish line ahead of me, and I thought I might have to sit down and not finish! I have to admit, I did get a little choked up when I crossed the finish line, and I felt really proud of myself for living with Crohn’s disease, yet still living my life to the fullest even after surgery to remove a portion of my small and large intestine.
She is still trying to make her fundraising goal—with an extension until August 21st.
The website address for on-line donations is: http://www.active.com/donations/fundraise_public.cfm?ckey=napaNE13&force_a2=y&key=TCNE_Napa13DCummin1
Donations can still be made using this website,
or a check made out to CCFA can be mailed to her
at 34 Miller Road, Brattleboro, Vermont 05301.
 A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
A New Diet…. Begun just over four weeks ago, is really helping! I am inspired by my friend, and fellow Crohnie, Katy Haldiman, RN, MS, The Paleo Nurse, and my consultants, Jordon Reasoner, and Steve Wright of SCD Lifestyle, to try a simplified diet to help my recent recurrence of Crohn’s from spreading.
Crohn’s is not easily deterred. I was so lucky to have seven years of clinical remission. It was only in the last year, that my disease spread. My last seven years have been filled with hope and health, and it is easy to fall into despair when the doctors tell you that your disease has gone from nonexistent to “severe.”
~
Rather than saying “Woe is me,” and spending time feeling sad and useless (I did a lot of that, believe me), I decided to take action, and try to live the words of the Dalai Lama:
“Scientists say that a healthy mind is a major factor for a healthy body,” His Holiness said. “If you’re serious about your health, think and take most concern for your peace of mind. That’s very, very important.”
That said, I am on my way to health, for sure—no time to sit on my cushion meditating (I do that daily for a few minutes still); rather, I need to stay focused and take care of my body: better food, sleep, stress relief, education, awareness, team building, satisfying work, making money enough to live on, giving back to my community and the world…working for peace, justice, and environmental sustainability. According to His Holiness the XIV Dalai Lama, peace of mind is essential for health—words to live by.
This new diet, very much like The Paleo, is giving me strength and vitality. It is not for everyone—and I always tell people you must proceed with a doctor’s knowledge, for Crohn’s and UC can be serious, even fatal, if not managed correctly. I have worked really hard to form a collaborative team—my own book’s co-author, Jessica Black, ND, is my stalwart supporter and her book, The Anti-Inflammation Diet and Recipe Book has just come it in a second edition and has sold almost 100,000 copies! Jessie is an amazing health practitioner.
~
I have eliminated ALL grains and dairy from my diet—woohoo! What a difference. I found this great site, and I can use almond meal flour (also coconut flour), and I eat fruits and veggies, nuts and animal protein pretty much non-stop. I had an adjustment for the first week, as I really missed my oatmeal in the morning, but as you can see from the photo, my morning meal is wonderful and tasty, too.
I hope this post inspires people to look at their own diets, and proceed with caution (this diet is not recommended if you have flare-up symptoms of Crohn’s or ulcerative colitis). I began this diet with no symptoms, and after the first week, I started to feel like I had more energy, and my stress levels are kept low by walking 4 miles a day and sleeping 8 hours per night.
I’ll post some more photos of my wonderful meals… Summer is the best time to do this diet: only organic fruits and veggies and meat must be antibiotic-free, grass-fed…that whole thing! I buy all local meat, eggs, fruits and veggies… And I plan on putting up and preserving a lot of them this summer so I can continue summer’s bounty from my freezer (and canning room) during the cold Vermont winter!
I also have a nice little garden growing…. Kale, and more kale! Plus, tomatoes, green beans, lettuce, spinach, onions, asparagus, etc. growing your own food is another way to reduce stress and get physically fit—gardening is good for upper body strength!